Monday Poster Session
Category: Stomach
P3354 - Finding a Gastroduodenal Fistula
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Ethan Chambers, MS, MD
Norwalk Hospital
Fairfield, CT
Presenting Author(s)
Ethan Chambers, MS, MD1, Gurjeet Judge, MD2, Robert Lam, MD3, Kenneth Hung, MD, MPH4
1Norwalk Hospital, Fairfield, CT; 2Norwalk Hospital, Norwalk, CT; 3Yale Digestive Diseases, New Haven, CT; 4Yale School of Medicine, New Haven, CT
Introduction: Gastroduodenal fistula (GDF), also referred to as double pylorus (DP), is an uncommon condition that may arise congenitally from abnormalities in gastrointestinal duplication or more frequently as a secondary condition due to peptic ulcer disease. Research indicates it is detected in approximately 0.001% to 0.4% of upper gastrointestinal tract endoscopies, with a higher prevalence observed among males [1].
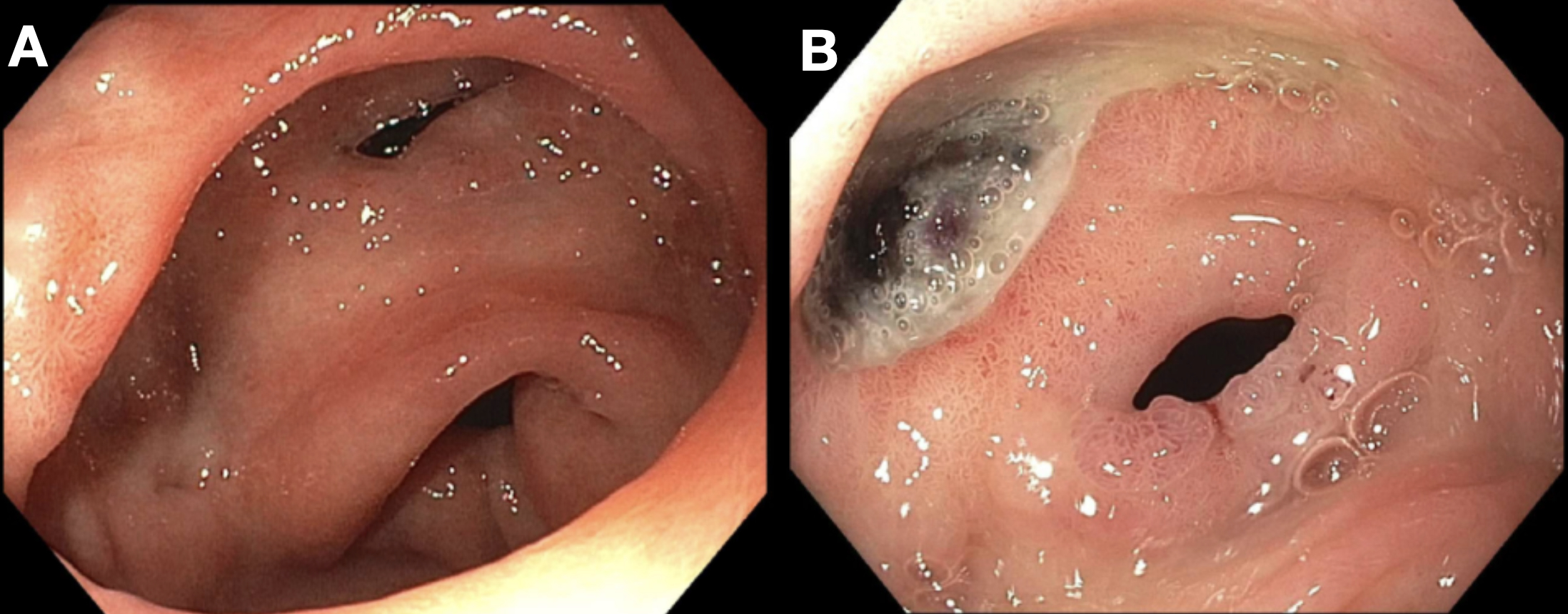
Case Description/Methods: A 66-year-old female with a medical history of recurrent peptic ulcer disease, chronic pancreatitis, COPD and hypertension presented to the hospital with abdominal pain, nausea and vomiting lasting four days. She reported several episodes of non-bloody vomiting progressing to small amounts of hematemesis. Additionally, she had two episodes of black, tarry stool the day before admission. During upper gastrointestinal endoscopy (EGD), findings included a small hiatal hernia, gastric erosions without signs of active bleeding, and the recognition of a previously reported gastric-duodenal bulb fistula located in the pre-pyloric region. The fistula's opening was slightly larger than 1 cm in diameter, allowing easy passage of the endoscope into the duodenal bulb. Pathological examination revealed mild chronic inactive gastritis and tested negative for H. pylori.
Discussion: It is hypothesized that GDF forms as an accessory pyloric channel when a peptic ulcer penetrates from the stomach to the first part of the duodenum and re-epithelizes. This process creates an additional pathway between these digestive structures [2]. GDF typically presents without symptoms; however, individuals may experience a spectrum of manifestations from mild indigestion to more serious complications such as gastrointestinal bleeding [3], as seen with our patient. Alternatively, GDF can also be congenital, where gastrointestinal bleeding seems to occur coincidentally. According to the literature, congenital DP is attributed to a tubular duplication of the pylorus [4]. Regarding treatment, GDF typically does not necessitate surgical or endoscopic intervention unless symptoms persist despite medical therapy or in situations involving recurrent bleeding, obstruction, or perforation [5].
Disclosures:
Ethan Chambers, MS, MD1, Gurjeet Judge, MD2, Robert Lam, MD3, Kenneth Hung, MD, MPH4. P3354 - Finding a Gastroduodenal Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Norwalk Hospital, Fairfield, CT; 2Norwalk Hospital, Norwalk, CT; 3Yale Digestive Diseases, New Haven, CT; 4Yale School of Medicine, New Haven, CT
Introduction: Gastroduodenal fistula (GDF), also referred to as double pylorus (DP), is an uncommon condition that may arise congenitally from abnormalities in gastrointestinal duplication or more frequently as a secondary condition due to peptic ulcer disease. Research indicates it is detected in approximately 0.001% to 0.4% of upper gastrointestinal tract endoscopies, with a higher prevalence observed among males [1].
Case Description/Methods: A 66-year-old female with a medical history of recurrent peptic ulcer disease, chronic pancreatitis, COPD and hypertension presented to the hospital with abdominal pain, nausea and vomiting lasting four days. She reported several episodes of non-bloody vomiting progressing to small amounts of hematemesis. Additionally, she had two episodes of black, tarry stool the day before admission. During upper gastrointestinal endoscopy (EGD), findings included a small hiatal hernia, gastric erosions without signs of active bleeding, and the recognition of a previously reported gastric-duodenal bulb fistula located in the pre-pyloric region. The fistula's opening was slightly larger than 1 cm in diameter, allowing easy passage of the endoscope into the duodenal bulb. Pathological examination revealed mild chronic inactive gastritis and tested negative for H. pylori.
Discussion: It is hypothesized that GDF forms as an accessory pyloric channel when a peptic ulcer penetrates from the stomach to the first part of the duodenum and re-epithelizes. This process creates an additional pathway between these digestive structures [2]. GDF typically presents without symptoms; however, individuals may experience a spectrum of manifestations from mild indigestion to more serious complications such as gastrointestinal bleeding [3], as seen with our patient. Alternatively, GDF can also be congenital, where gastrointestinal bleeding seems to occur coincidentally. According to the literature, congenital DP is attributed to a tubular duplication of the pylorus [4]. Regarding treatment, GDF typically does not necessitate surgical or endoscopic intervention unless symptoms persist despite medical therapy or in situations involving recurrent bleeding, obstruction, or perforation [5].
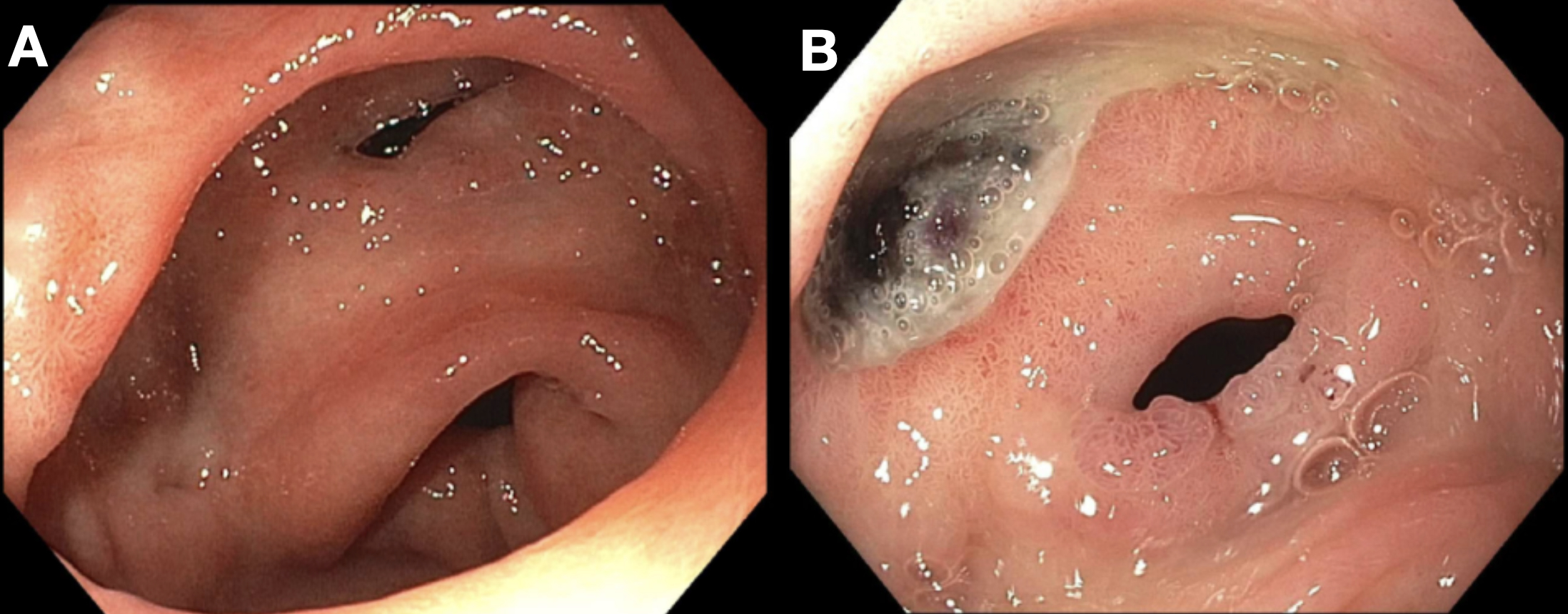
Figure: pre-pyloric stomach (A and B) with a fistula between the antrum and the duodenal bulb.
Disclosures:
Ethan Chambers indicated no relevant financial relationships.
Gurjeet Judge indicated no relevant financial relationships.
Robert Lam indicated no relevant financial relationships.
Kenneth Hung indicated no relevant financial relationships.
Ethan Chambers, MS, MD1, Gurjeet Judge, MD2, Robert Lam, MD3, Kenneth Hung, MD, MPH4. P3354 - Finding a Gastroduodenal Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
