Monday Poster Session
Category: Stomach
P3355 - A Patient With Recurrent Gastric Erosions and Ulcers and the Underappreciation of Gastric Ischemia
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Arman Maqsudlu, MD
Cooper University Hospital
Camden, NJ
Presenting Author(s)
Arman Maqsudlu, MD1, Daniel Garrido, MD1, Krysta Contino, MD2
1Cooper University Hospital, Camden, NJ; 2Digestive Health Institute at Cooper University Hospital, Mount Laurel, NJ
Introduction: Gastric ischemia is uncommon due to the rich collateral vascular supply of the stomach. Acute ischemic symptoms include nausea/vomiting, abdominal pain, bloating/distention, and upper gastrointestinal (GI) bleeding, while chronic ischemic symptoms may also include anemia, diarrhea, and gastroparesis. Gastric ischemia is often underdiagnosed until complications arise. Here we present a patient with chronic gastric ischemia diagnosed after identification of mucosal changes seen on esophagogastroduodenoscopy (EGD).
Case Description/Methods: A 76-year-old female with a history of type 2 diabetes, chronic kidney disease (CKD), gastroparesis, obesity, metabolic dysfunction-associated steatotic liver disease (MASLD), and gastric ulcers and presented in 09/2022 with chronic nausea and epigastric pain. This was initially believed to be secondary to gastroparesis. She was also on sucralfate and a proton-pump inhibitor for her history of ulcers. She subsequently underwent two separate EGDs in 11/2022 and 02/2023, with the former finding a non-bleeding esophageal ulcer near the gastroesophageal junction and the latter demonstrating three oozing superficial ulcers in the gastric antrum. All biopsies were negative for Helicobacter pylori. Zollinger-Ellison syndrome was ruled unlikely due to gastric pH of 7 seen during EGD and gastrin level less than 1000 (284). Follow-up EGD in 04/2023 showed one non-bleeding superficial ulcer with a few dispersed erosions in the gastric antrum, but there were also areas of white-colored mucosa present after insufflation. Biopsies were unremarkable. An MR Angiography of the Abdomen/Pelvis was ordered with contrast to evaluate for potential ischemia, which revealed severe stenosis at the origin of the celiac artery with associated plaque. The patient followed with vascular surgery who recommended further imaging with CT Angiography.
Discussion: It is critical to identify gastric ischemia due to the high risk of morbidity and mortality. Acute gastric distention can cause or exacerbate ischemia. Ischemia can also impair gastric motility leading to a cycle of worsening distention and ischemia. Patients with gastroparesis may be at greater risk for complications without further intervention aimed at correcting the etiology of the underlying ischemia. The most notable complication from this is gastric perforation, which has a significantly high morbidity and mortality. Accurate diagnosis is imperative to improve patient outcomes.

Disclosures:
Arman Maqsudlu, MD1, Daniel Garrido, MD1, Krysta Contino, MD2. P3355 - A Patient With Recurrent Gastric Erosions and Ulcers and the Underappreciation of Gastric Ischemia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cooper University Hospital, Camden, NJ; 2Digestive Health Institute at Cooper University Hospital, Mount Laurel, NJ
Introduction: Gastric ischemia is uncommon due to the rich collateral vascular supply of the stomach. Acute ischemic symptoms include nausea/vomiting, abdominal pain, bloating/distention, and upper gastrointestinal (GI) bleeding, while chronic ischemic symptoms may also include anemia, diarrhea, and gastroparesis. Gastric ischemia is often underdiagnosed until complications arise. Here we present a patient with chronic gastric ischemia diagnosed after identification of mucosal changes seen on esophagogastroduodenoscopy (EGD).
Case Description/Methods: A 76-year-old female with a history of type 2 diabetes, chronic kidney disease (CKD), gastroparesis, obesity, metabolic dysfunction-associated steatotic liver disease (MASLD), and gastric ulcers and presented in 09/2022 with chronic nausea and epigastric pain. This was initially believed to be secondary to gastroparesis. She was also on sucralfate and a proton-pump inhibitor for her history of ulcers. She subsequently underwent two separate EGDs in 11/2022 and 02/2023, with the former finding a non-bleeding esophageal ulcer near the gastroesophageal junction and the latter demonstrating three oozing superficial ulcers in the gastric antrum. All biopsies were negative for Helicobacter pylori. Zollinger-Ellison syndrome was ruled unlikely due to gastric pH of 7 seen during EGD and gastrin level less than 1000 (284). Follow-up EGD in 04/2023 showed one non-bleeding superficial ulcer with a few dispersed erosions in the gastric antrum, but there were also areas of white-colored mucosa present after insufflation. Biopsies were unremarkable. An MR Angiography of the Abdomen/Pelvis was ordered with contrast to evaluate for potential ischemia, which revealed severe stenosis at the origin of the celiac artery with associated plaque. The patient followed with vascular surgery who recommended further imaging with CT Angiography.
Discussion: It is critical to identify gastric ischemia due to the high risk of morbidity and mortality. Acute gastric distention can cause or exacerbate ischemia. Ischemia can also impair gastric motility leading to a cycle of worsening distention and ischemia. Patients with gastroparesis may be at greater risk for complications without further intervention aimed at correcting the etiology of the underlying ischemia. The most notable complication from this is gastric perforation, which has a significantly high morbidity and mortality. Accurate diagnosis is imperative to improve patient outcomes.

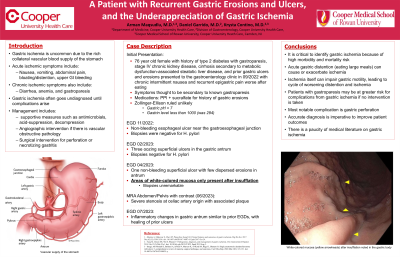
Figure: White-colored mucosa (yellow arrowheads) after insufflation noted in the gastric body.
Disclosures:
Arman Maqsudlu indicated no relevant financial relationships.
Daniel Garrido indicated no relevant financial relationships.
Krysta Contino indicated no relevant financial relationships.
Arman Maqsudlu, MD1, Daniel Garrido, MD1, Krysta Contino, MD2. P3355 - A Patient With Recurrent Gastric Erosions and Ulcers and the Underappreciation of Gastric Ischemia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
