Monday Poster Session
Category: Stomach
P3360 - Buried Bumper Syndrome: A Rare Complication of Percutaneous Endoscopic Gastrostomy Tube
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Omer Usman, MD
Texas Tech University Health Sciences Center
El Paso, TX
Presenting Author(s)
Omer Usman, MD1, Muhammad Waqas Khan, MBBS2, Muhammad Usman Shahbaz, MBBS3, Muhammad Ali Hassan, MBBS4, Osama Ijaz, MBBS2, Zoha Shahzad, MBBS5, Maryam Abbas Malik, MBBS2
1Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, TX; 2Services Institute of Medical Sciences, Lahore, Punjab, Pakistan; 3Jinnah Hospital, Lahore, Punjab, Pakistan; 4Shifa College of Medicine, Islamabad, Islamabad, Pakistan; 5Fatima Jinnah Medical University, Lahore, Punjab, Pakistan
Introduction: Percutaneous endoscopic gastrostomy (PEG) tube placement is a preferred method for providing long-term nutritional support in patients with significant feeding difficulties. Buried bumper syndrome (BBS) is a rare but serious complication, characterized by the migration of the internal bumper of the PEG tube into the gastric or abdominal wall, leading to potentially life-threatening consequences. The incidence of BBS ranges from 0.3% to 2.4% per year in PEG tube patients. We present a case of a 79-year-old female with a history of squamous cell carcinoma of the upper esophagus that developed acute BBS following PEG tube placement.
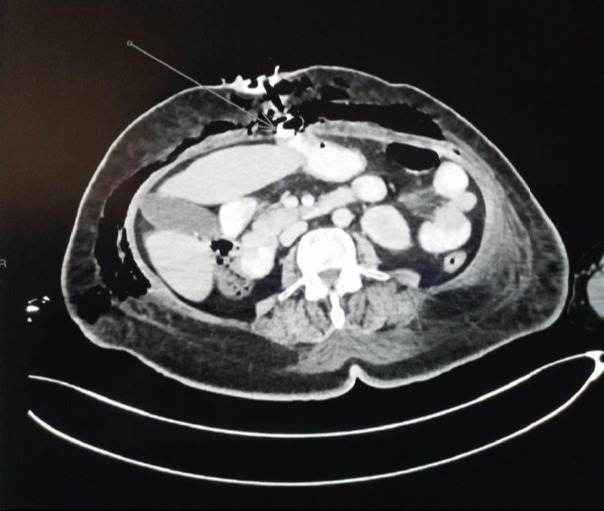
Case Description/Methods: A 79-year-old female with a medical history of type-II diabetes mellitus and squamous cell carcinoma of the upper esophagus, for which she had undergone surgical resection followed by radical chemotherapy and radiotherapy, presented to the emergency department with complaints of abdominal pain and fever seven days after PEG tube insertion. On physical examination, she was found to be hypotensive and tachycardic, with marked tenderness and crepitus in the left hypochondrium and around the PEG tube insertion site. A CT scan revealed the dislodgement of the internal bumper of the PEG tube, resulting in subcutaneous emphysema along the abdominal wall. The displaced PEG tube was subsequently removed, and surgical debridement was performed. The patient was managed in the intensive care unit due to severe sepsis but stabilized after four days. A new PEG tube was placed to ensure adequate long-term nutritional support. The patient tolerated tube feeds well postoperatively without further complications.
Discussion: Buried bumper syndrome, while uncommon, can lead to severe complications such as subcutaneous emphysema, sepsis, and tissue necrosis. Early diagnosis is essential and can be effectively achieved through imaging studies, with CT scans being particularly useful. Prompt recognition and timely surgical intervention are critical to manage this condition and prevent further morbidity. A multidisciplinary approach involving gastroenterologists, surgeons, and critical care specialists is vital for the successful management of BBS and ensuring optimal patient outcomes. Our case highlights the importance of coordinated care and vigilance in monitoring for PEG tube-related complications.
Disclosures:
Omer Usman, MD1, Muhammad Waqas Khan, MBBS2, Muhammad Usman Shahbaz, MBBS3, Muhammad Ali Hassan, MBBS4, Osama Ijaz, MBBS2, Zoha Shahzad, MBBS5, Maryam Abbas Malik, MBBS2. P3360 - Buried Bumper Syndrome: A Rare Complication of Percutaneous Endoscopic Gastrostomy Tube, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, TX; 2Services Institute of Medical Sciences, Lahore, Punjab, Pakistan; 3Jinnah Hospital, Lahore, Punjab, Pakistan; 4Shifa College of Medicine, Islamabad, Islamabad, Pakistan; 5Fatima Jinnah Medical University, Lahore, Punjab, Pakistan
Introduction: Percutaneous endoscopic gastrostomy (PEG) tube placement is a preferred method for providing long-term nutritional support in patients with significant feeding difficulties. Buried bumper syndrome (BBS) is a rare but serious complication, characterized by the migration of the internal bumper of the PEG tube into the gastric or abdominal wall, leading to potentially life-threatening consequences. The incidence of BBS ranges from 0.3% to 2.4% per year in PEG tube patients. We present a case of a 79-year-old female with a history of squamous cell carcinoma of the upper esophagus that developed acute BBS following PEG tube placement.
Case Description/Methods: A 79-year-old female with a medical history of type-II diabetes mellitus and squamous cell carcinoma of the upper esophagus, for which she had undergone surgical resection followed by radical chemotherapy and radiotherapy, presented to the emergency department with complaints of abdominal pain and fever seven days after PEG tube insertion. On physical examination, she was found to be hypotensive and tachycardic, with marked tenderness and crepitus in the left hypochondrium and around the PEG tube insertion site. A CT scan revealed the dislodgement of the internal bumper of the PEG tube, resulting in subcutaneous emphysema along the abdominal wall. The displaced PEG tube was subsequently removed, and surgical debridement was performed. The patient was managed in the intensive care unit due to severe sepsis but stabilized after four days. A new PEG tube was placed to ensure adequate long-term nutritional support. The patient tolerated tube feeds well postoperatively without further complications.
Discussion: Buried bumper syndrome, while uncommon, can lead to severe complications such as subcutaneous emphysema, sepsis, and tissue necrosis. Early diagnosis is essential and can be effectively achieved through imaging studies, with CT scans being particularly useful. Prompt recognition and timely surgical intervention are critical to manage this condition and prevent further morbidity. A multidisciplinary approach involving gastroenterologists, surgeons, and critical care specialists is vital for the successful management of BBS and ensuring optimal patient outcomes. Our case highlights the importance of coordinated care and vigilance in monitoring for PEG tube-related complications.
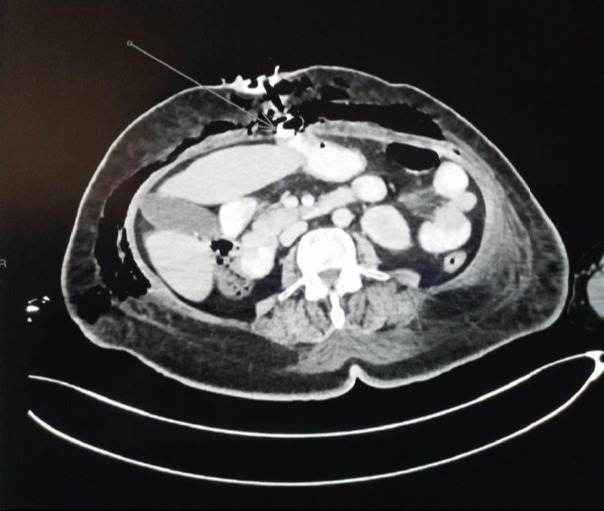
Figure: CT Abdomen and pelvis with contrast shows dislodgement of the internal bumper of the PEG tube, resulting in subcutaneous emphysema along the abdominal walls
Disclosures:
Omer Usman indicated no relevant financial relationships.
Muhammad Waqas Khan indicated no relevant financial relationships.
Muhammad Usman Shahbaz indicated no relevant financial relationships.
Muhammad Ali Hassan indicated no relevant financial relationships.
Osama Ijaz indicated no relevant financial relationships.
Zoha Shahzad indicated no relevant financial relationships.
Maryam Abbas Malik indicated no relevant financial relationships.
Omer Usman, MD1, Muhammad Waqas Khan, MBBS2, Muhammad Usman Shahbaz, MBBS3, Muhammad Ali Hassan, MBBS4, Osama Ijaz, MBBS2, Zoha Shahzad, MBBS5, Maryam Abbas Malik, MBBS2. P3360 - Buried Bumper Syndrome: A Rare Complication of Percutaneous Endoscopic Gastrostomy Tube, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
