Monday Poster Session
Category: Stomach
P3361 - Ischemic Gastritis: A Case Report and Review of Its Management
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Omer Usman, MD
Texas Tech University Health Sciences Center
El Paso, TX
Presenting Author(s)
Omer Usman, MD1, Barney Soskin, MD1, Swathi Veliginti, MD1, Muhammad Waqas Khan, MBBS2, Obaid Ur Rehman, MBBS2, Eeshal Fatima, MBBS2
1Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, TX; 2Services Institute of Medical Sciences, Lahore, Punjab, Pakistan
Introduction: The stomach has a rich blood supply consisting of 12 arteries, reducing the likelihood of ischemia. However, certain endoscopic procedures, medications, and atherosclerotic diseases have been documented to contribute to ischemic gastritis. We present a rare case of ischemic gastritis in an 82-year-old man with a significant medical history, including diabetes mellitus type 2, hypertension, stroke, coronary artery disease, and deep vein thrombosis.
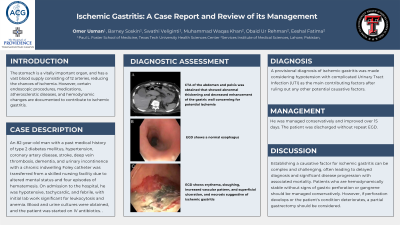
Case Description/Methods: An 82-year-old man with a past medical history of type 2 diabetes mellitus, hypertension, coronary artery disease, stroke, deep vein thrombosis, dementia, and urinary incontinence with a chronic indwelling Foley catheter was transferred from a skilled nursing facility due to altered mental status and four episodes of hematemesis. On admission to the hospital, he was hypotensive, tachycardic, and febrile, with initial lab work significant for leukocytosis and anemia with a normal coagulation profile. Blood and urine cultures were obtained, and the patient was started on IV antibiotics. Computed Tomography Angiography (CTA) of the abdomen revealed abnormal thickening and decreased enhancement of the gastric wall with marked mural edema, concerning potential ischemia. Esophagogastroduodenoscopy (EGD) showed a normal esophagus, while the mucosa of the gastric fundus and body exhibited erythema, sloughing, superficial ulceration, and an increased vascular pattern, indicating ischemic gastritis. A provisional diagnosis of ischemic gastritis was made, with the causative etiology determined to be hypotension secondary to a urinary tract infection (UTI) because the patient didn't have recent corrosive intake, medication changes, recent endoscopic procedures, or extensive atherosclerotic disease. The patient was managed conservatively and showed improvement over fifteen days. He was subsequently discharged without a repeat EGD.
Discussion: Establishing a causative factor for ischemic gastritis can be complex and challenging, often leading to delayed diagnosis and significant disease progression with associated mortality. Moderate hypotension in the absence of septic shock can also contribute to ischemic gastritis as in our case. Patients who are hemodynamically stable without signs of gastric perforation or gangrene should be managed conservatively. However, if perforation develops or the patient’s condition deteriorates, a partial gastrectomy should be considered.

Disclosures:
Omer Usman, MD1, Barney Soskin, MD1, Swathi Veliginti, MD1, Muhammad Waqas Khan, MBBS2, Obaid Ur Rehman, MBBS2, Eeshal Fatima, MBBS2. P3361 - Ischemic Gastritis: A Case Report and Review of Its Management, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, TX; 2Services Institute of Medical Sciences, Lahore, Punjab, Pakistan
Introduction: The stomach has a rich blood supply consisting of 12 arteries, reducing the likelihood of ischemia. However, certain endoscopic procedures, medications, and atherosclerotic diseases have been documented to contribute to ischemic gastritis. We present a rare case of ischemic gastritis in an 82-year-old man with a significant medical history, including diabetes mellitus type 2, hypertension, stroke, coronary artery disease, and deep vein thrombosis.
Case Description/Methods: An 82-year-old man with a past medical history of type 2 diabetes mellitus, hypertension, coronary artery disease, stroke, deep vein thrombosis, dementia, and urinary incontinence with a chronic indwelling Foley catheter was transferred from a skilled nursing facility due to altered mental status and four episodes of hematemesis. On admission to the hospital, he was hypotensive, tachycardic, and febrile, with initial lab work significant for leukocytosis and anemia with a normal coagulation profile. Blood and urine cultures were obtained, and the patient was started on IV antibiotics. Computed Tomography Angiography (CTA) of the abdomen revealed abnormal thickening and decreased enhancement of the gastric wall with marked mural edema, concerning potential ischemia. Esophagogastroduodenoscopy (EGD) showed a normal esophagus, while the mucosa of the gastric fundus and body exhibited erythema, sloughing, superficial ulceration, and an increased vascular pattern, indicating ischemic gastritis. A provisional diagnosis of ischemic gastritis was made, with the causative etiology determined to be hypotension secondary to a urinary tract infection (UTI) because the patient didn't have recent corrosive intake, medication changes, recent endoscopic procedures, or extensive atherosclerotic disease. The patient was managed conservatively and showed improvement over fifteen days. He was subsequently discharged without a repeat EGD.
Discussion: Establishing a causative factor for ischemic gastritis can be complex and challenging, often leading to delayed diagnosis and significant disease progression with associated mortality. Moderate hypotension in the absence of septic shock can also contribute to ischemic gastritis as in our case. Patients who are hemodynamically stable without signs of gastric perforation or gangrene should be managed conservatively. However, if perforation develops or the patient’s condition deteriorates, a partial gastrectomy should be considered.

Figure: A: CTA of the abdomen and pelvis was obtained that showed abnormal thickening and decreased enhancement of the gastric wall concerning for potential ischemia; B: EGD shows a normal esophagus; C: EGD shows erythema, sloughing, increased vascular pattern, and superficial ulceration, and necrosis suggestive of ischemic gastritis
Disclosures:
Omer Usman indicated no relevant financial relationships.
Barney Soskin indicated no relevant financial relationships.
Swathi Veliginti indicated no relevant financial relationships.
Muhammad Waqas Khan indicated no relevant financial relationships.
Obaid Ur Rehman indicated no relevant financial relationships.
Eeshal Fatima indicated no relevant financial relationships.
Omer Usman, MD1, Barney Soskin, MD1, Swathi Veliginti, MD1, Muhammad Waqas Khan, MBBS2, Obaid Ur Rehman, MBBS2, Eeshal Fatima, MBBS2. P3361 - Ischemic Gastritis: A Case Report and Review of Its Management, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
