Monday Poster Session
Category: Stomach
P3363 - Pembrolizumab Associated Severe Immune Checkpoint Inhibitor Gastritis Mimicking Gastric Outlet Obstruction
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Vivian Lee, MD
Kaiser Permanente
Los Angeles, CA
Presenting Author(s)
Vivian Lee, MD, Aviv Hever, MD, Christine Yu, MD
Kaiser Permanente, Los Angeles, CA
Introduction: Use of immune checkpoint inhibitors (ICIs) for cancer is increasing. Colonic inflammation is a well described immune-related adverse event (irAEs); however, gastritis is infrequently seen. We report an unusual case of ICI associated gastritis mimicking gastric outlet obstruction.
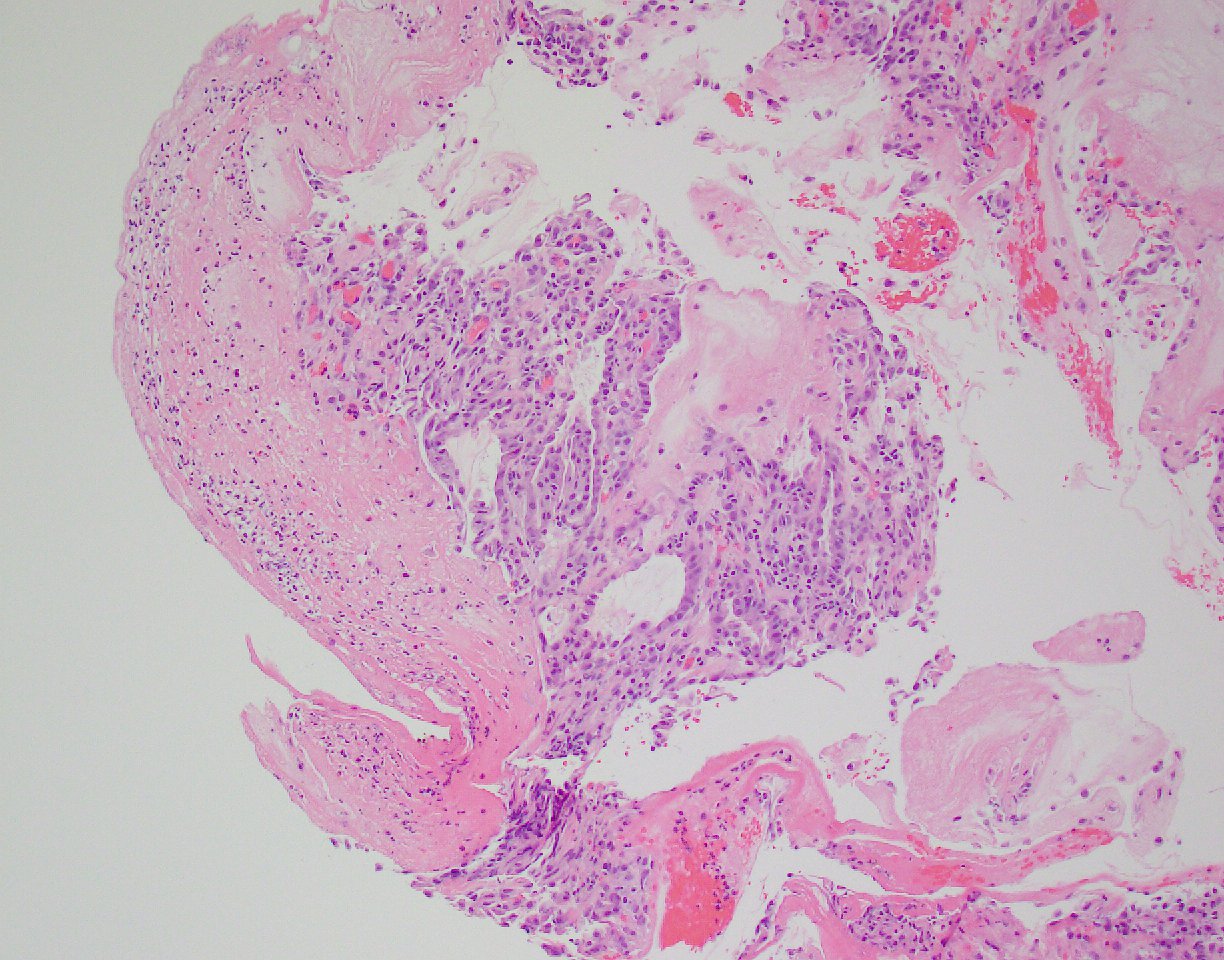
Case Description/Methods: A 59 year old male with auricular Merkel cell carcinoma with dermal metastases on pembrolizumab presented to the emergency room with postprandial epigastric pain, early satiety, nausea, vomiting and 20-pound weight loss. A CT scan showed multiple loops of nondilated small bowel in the right lower and middle abdomen, with diffusely thick walls and mucosal hyperenhancement consistent with enteritis. Follow up endoscopy revealed hemorrhagic gastropathy along the gastric body, incisura, and antrum. The endoscope was unable to traverse the pylorus, suggestive of gastric outlet obstruction. Pathology demonstrated surface ulceration, acute inflammation, and reactive epithelial atypia and in the setting of pembrolizumab, were secondary to ICI associated gastritis. Pembrolizumab was discontinued. The patient underwent nasogastric tube decompression and was started on IV methylprednisolone with clinical improvement over several days. His diet was advanced and he was transitioned to a prednisone taper. He was seen in oncology follow-up with complete resolution of symptoms.
Discussion: ICI associated gastritis can occur at any time during use of ICIs and is diagnosed based on a combination of clinical symptoms with endoscopic and histopathological findings. While isolated ICI gastritis has been described, concurrent enteritis or colitis is more common. Symptoms include nausea, vomiting, early satiety, weight loss, or even gastric outlet obstruction as seen in our case. Endoscopic characteristics are network-pattern erosion, ulceration, erythema, and edematous mucosa with friability. Histopathological findings are non-specific, including intraepithelial lymphocytosis, fibrinopurulent exudate, apoptosis, or epithalaxia. Discontinuation of ICIs and treatment with steroids frequently lead to rapid improvement in symptoms after several days. Prior literature shows that patients with concomitant enteritis or colitis were more likely to need steroids or stop ICI therapy. As the use of these agents become more frequent, recognition of irAEs is imperative. Endoscopic and histologic findings are non-specific and a high clinical suspicion is needed for early detection and management of ICI-associated gastritis.
Disclosures:
Vivian Lee, MD, Aviv Hever, MD, Christine Yu, MD. P3363 - Pembrolizumab Associated Severe Immune Checkpoint Inhibitor Gastritis Mimicking Gastric Outlet Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Kaiser Permanente, Los Angeles, CA
Introduction: Use of immune checkpoint inhibitors (ICIs) for cancer is increasing. Colonic inflammation is a well described immune-related adverse event (irAEs); however, gastritis is infrequently seen. We report an unusual case of ICI associated gastritis mimicking gastric outlet obstruction.
Case Description/Methods: A 59 year old male with auricular Merkel cell carcinoma with dermal metastases on pembrolizumab presented to the emergency room with postprandial epigastric pain, early satiety, nausea, vomiting and 20-pound weight loss. A CT scan showed multiple loops of nondilated small bowel in the right lower and middle abdomen, with diffusely thick walls and mucosal hyperenhancement consistent with enteritis. Follow up endoscopy revealed hemorrhagic gastropathy along the gastric body, incisura, and antrum. The endoscope was unable to traverse the pylorus, suggestive of gastric outlet obstruction. Pathology demonstrated surface ulceration, acute inflammation, and reactive epithelial atypia and in the setting of pembrolizumab, were secondary to ICI associated gastritis. Pembrolizumab was discontinued. The patient underwent nasogastric tube decompression and was started on IV methylprednisolone with clinical improvement over several days. His diet was advanced and he was transitioned to a prednisone taper. He was seen in oncology follow-up with complete resolution of symptoms.
Discussion: ICI associated gastritis can occur at any time during use of ICIs and is diagnosed based on a combination of clinical symptoms with endoscopic and histopathological findings. While isolated ICI gastritis has been described, concurrent enteritis or colitis is more common. Symptoms include nausea, vomiting, early satiety, weight loss, or even gastric outlet obstruction as seen in our case. Endoscopic characteristics are network-pattern erosion, ulceration, erythema, and edematous mucosa with friability. Histopathological findings are non-specific, including intraepithelial lymphocytosis, fibrinopurulent exudate, apoptosis, or epithalaxia. Discontinuation of ICIs and treatment with steroids frequently lead to rapid improvement in symptoms after several days. Prior literature shows that patients with concomitant enteritis or colitis were more likely to need steroids or stop ICI therapy. As the use of these agents become more frequent, recognition of irAEs is imperative. Endoscopic and histologic findings are non-specific and a high clinical suspicion is needed for early detection and management of ICI-associated gastritis.
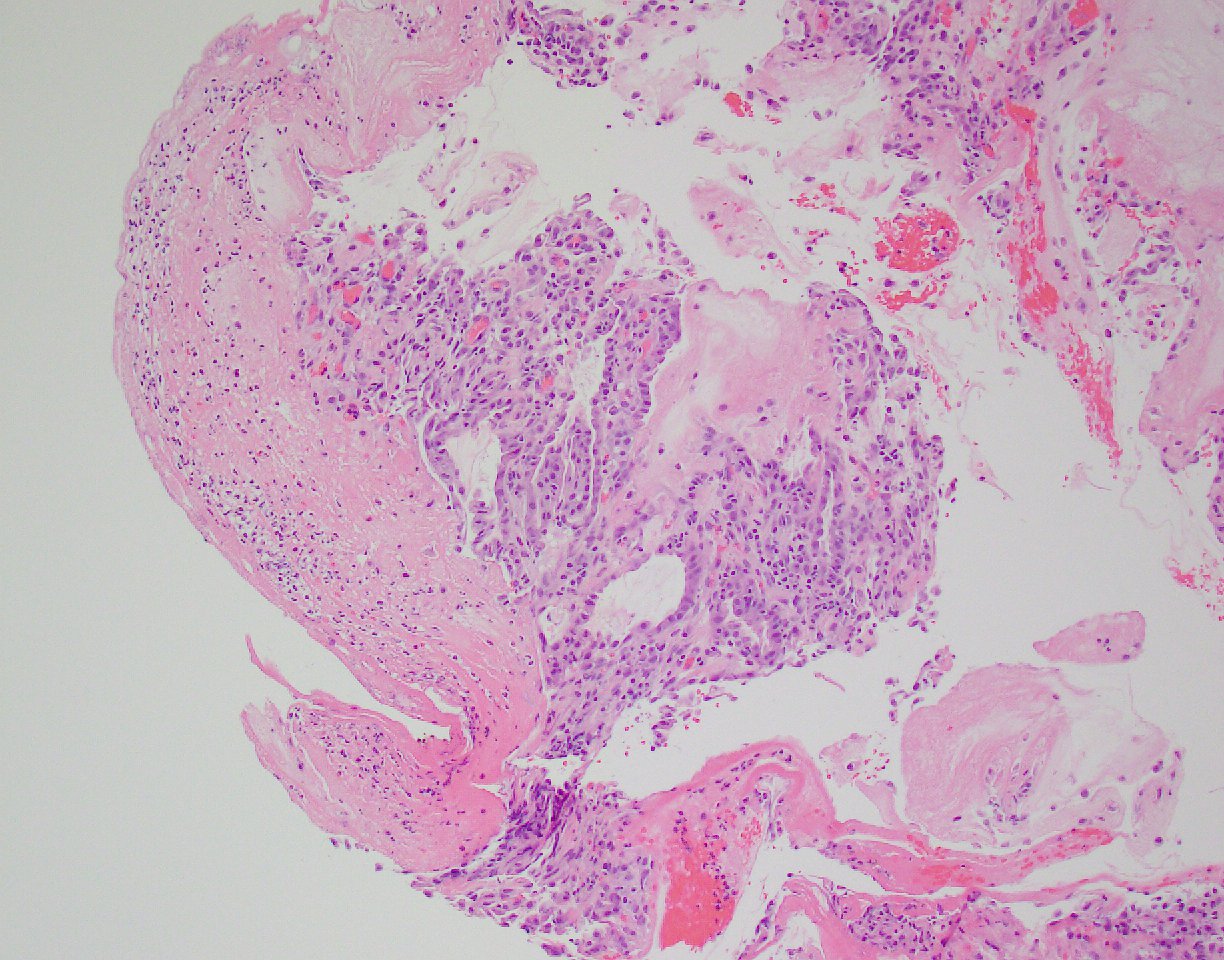
Figure: Histologic findings of gastric mucosa displaying surface ulceration, hemorrhage, acute inflammation, and reactive epithelial atypia.
Disclosures:
Vivian Lee indicated no relevant financial relationships.
Aviv Hever indicated no relevant financial relationships.
Christine Yu indicated no relevant financial relationships.
Vivian Lee, MD, Aviv Hever, MD, Christine Yu, MD. P3363 - Pembrolizumab Associated Severe Immune Checkpoint Inhibitor Gastritis Mimicking Gastric Outlet Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
