Monday Poster Session
Category: Small Intestine
P3266 - Severe Scleroderma Presenting With High Grade Distal Small Bowel Obstruction
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Natasha Mederos, MD
University of Miami Miller School of Medicine at Holy Cross Hospital, FL
Presenting Author(s)
Natasha Mederos, MD1, Mary Parianos, MD1, Katelyn Kaufman, DO2, Luis Penaranda, MD2
1University of Miami Miller School of Medicine at Holy Cross Hospital, Fort Lauderdale, FL; 2University of Miami, Fort Lauderdale, FL
Introduction: Systemic sclerosis (SSc) is a rare autoimmune disease characterized by fibroproliferative microvasculature alterations leading to fibrosis and loss of function of the skin and internal organs. Intestinal motility dysfunction is commonly reported in SSc, with 65% of patients being asymptomatic leading to an under-diagnosis or delayed diagnosis of small bowel involvement. Small bowel involvement in SSc can manifest as dysmotility secondary to poor smooth muscle activity and stiffness, leading to complications such as pseudo-obstruction, pneumatosis cystoides intestinalis, small intestinal bacterial overgrowth (SIBO), and diverticula.
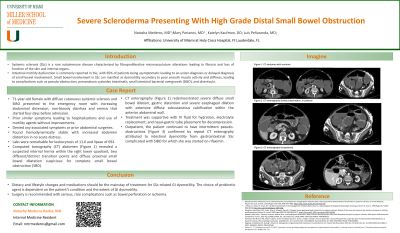
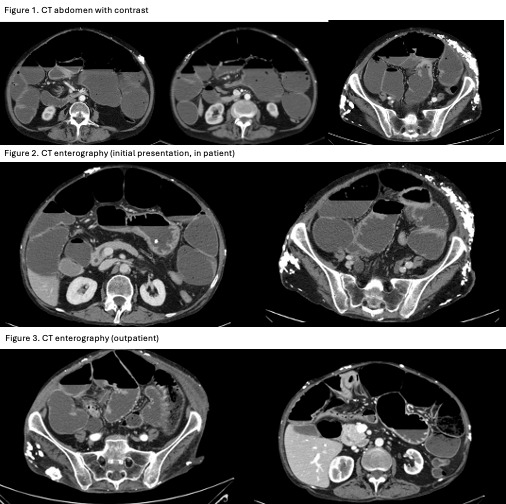
Case Description/Methods: A 71-year-old female with diffuse cutaneous systemic sclerosis and SIBO presented to the emergency room with increasing abdominal distension, non-bloody diarrhea and emesis that started four days before admission. Patient mentioned prior similar symptoms leading to hospitalizations and use of motility agents without improvements. Denied any associated symptoms or prior abdominal surgeries. On arrival, patient was found hemodynamically stable with increased abdomen distention in no acute distress. Labs were remarkable for leukocytosis of 11.6 and lipase of 692. Computed tomography (CT) abdomen (Figure 1) revealed a suspected internal hernia within the right lower quadrant, two different/distinct transition points and diffuse proximal small bowel dilatation suspicious for complete small bowel obstruction (SBO). CT enterography (Figure 2) redemonstrated severe diffuse small bowel dilation, gastric distention and severe esophageal dilation with extensive diffuse subcutaneous calcification within the anterior abdominal wall. Treatment was supportive with IV fluid for hydration, electrolyte replacement, and nasal-gastric tube placement for decompression. Outpatient, the patient continued to have intermittent pseudo-obstructions (Figure 3) confirmed by repeat CT enterogrphy attributed to intestinal dysmotility from gastrointestinal SSc complicated with SIBO for which she was started on rifaximin.
Discussion: Dietary and lifestyle changes and medications should be the mainstay of treatment for SSc-related GI dysmotility. The choice of prokinetic agent is dependent on the patient’s condition and the extent of GI dysmotility. Surgery is recommended with serious, rare complications such as bowel perforation or ischemia.
Disclosures:
Natasha Mederos, MD1, Mary Parianos, MD1, Katelyn Kaufman, DO2, Luis Penaranda, MD2. P3266 - Severe Scleroderma Presenting With High Grade Distal Small Bowel Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Miami Miller School of Medicine at Holy Cross Hospital, Fort Lauderdale, FL; 2University of Miami, Fort Lauderdale, FL
Introduction: Systemic sclerosis (SSc) is a rare autoimmune disease characterized by fibroproliferative microvasculature alterations leading to fibrosis and loss of function of the skin and internal organs. Intestinal motility dysfunction is commonly reported in SSc, with 65% of patients being asymptomatic leading to an under-diagnosis or delayed diagnosis of small bowel involvement. Small bowel involvement in SSc can manifest as dysmotility secondary to poor smooth muscle activity and stiffness, leading to complications such as pseudo-obstruction, pneumatosis cystoides intestinalis, small intestinal bacterial overgrowth (SIBO), and diverticula.
Case Description/Methods: A 71-year-old female with diffuse cutaneous systemic sclerosis and SIBO presented to the emergency room with increasing abdominal distension, non-bloody diarrhea and emesis that started four days before admission. Patient mentioned prior similar symptoms leading to hospitalizations and use of motility agents without improvements. Denied any associated symptoms or prior abdominal surgeries. On arrival, patient was found hemodynamically stable with increased abdomen distention in no acute distress. Labs were remarkable for leukocytosis of 11.6 and lipase of 692. Computed tomography (CT) abdomen (Figure 1) revealed a suspected internal hernia within the right lower quadrant, two different/distinct transition points and diffuse proximal small bowel dilatation suspicious for complete small bowel obstruction (SBO). CT enterography (Figure 2) redemonstrated severe diffuse small bowel dilation, gastric distention and severe esophageal dilation with extensive diffuse subcutaneous calcification within the anterior abdominal wall. Treatment was supportive with IV fluid for hydration, electrolyte replacement, and nasal-gastric tube placement for decompression. Outpatient, the patient continued to have intermittent pseudo-obstructions (Figure 3) confirmed by repeat CT enterogrphy attributed to intestinal dysmotility from gastrointestinal SSc complicated with SIBO for which she was started on rifaximin.
Discussion: Dietary and lifestyle changes and medications should be the mainstay of treatment for SSc-related GI dysmotility. The choice of prokinetic agent is dependent on the patient’s condition and the extent of GI dysmotility. Surgery is recommended with serious, rare complications such as bowel perforation or ischemia.
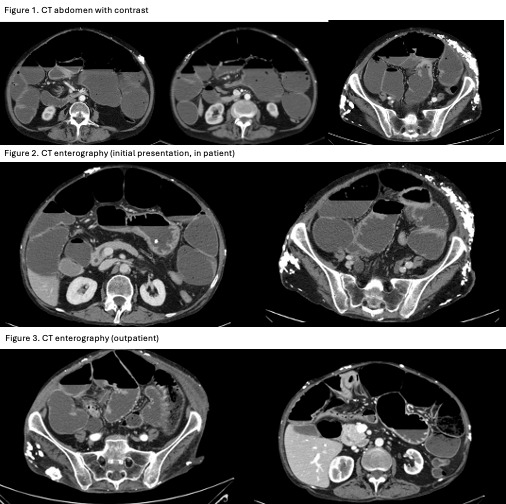
Figure: Figure 1. CT abomen w/ con (2023, inpatient) showing focal thickening of the proximal/mid jejunum resulting in proximal fluid-filled and dilated small bowel loops. Two different/distinct transition points, resulting in diffuse proximal small bowel dilatation.
Figure 2. CT enterography (2023; inpatient) redemonstrated severe diffuse small bowel dilation, gastric distention and severe esophageal dilation.
Figure 3. CT enterography (2024; outpatient) abnormal wall thickening of right upper quadrant of small bowel. Dilated loops of bowel with transition point in the right lower quadrant near ileocecal valve.
Figure 2. CT enterography (2023; inpatient) redemonstrated severe diffuse small bowel dilation, gastric distention and severe esophageal dilation.
Figure 3. CT enterography (2024; outpatient) abnormal wall thickening of right upper quadrant of small bowel. Dilated loops of bowel with transition point in the right lower quadrant near ileocecal valve.
Disclosures:
Natasha Mederos indicated no relevant financial relationships.
Mary Parianos indicated no relevant financial relationships.
Katelyn Kaufman indicated no relevant financial relationships.
Luis Penaranda indicated no relevant financial relationships.
Natasha Mederos, MD1, Mary Parianos, MD1, Katelyn Kaufman, DO2, Luis Penaranda, MD2. P3266 - Severe Scleroderma Presenting With High Grade Distal Small Bowel Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
