Monday Poster Session
Category: Small Intestine
P3277 - Duodenal Pyloric Gland Adenoma in an Immunocompromised Patient
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Adrienne M. Bielawski, MD
Montefiore Medical Center/Albert Einstein College of Medicine
Bronx, NY
Presenting Author(s)
Adrienne M. Bielawski, MD1, Amanda Rupert, MD2, Kuaybe Karakus Gulen, MD2, Frederick Yick, MD2
1Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, NY; 2Westchester Medical Center, Valhalla, NY
Introduction: A pyloric gland adenoma (PGA) is a rare neoplasm that can present as a duodenal non-ampullary polyp. PGAs can progress to invasive adenocarcinoma and should undergo resection and surveillance, although recurrence is rare. We report a case of an upper gastrointestinal bleed following resection of a duodenal polyp later identified as a PGA in an immunocompromised patient.
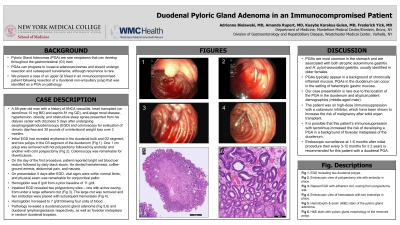
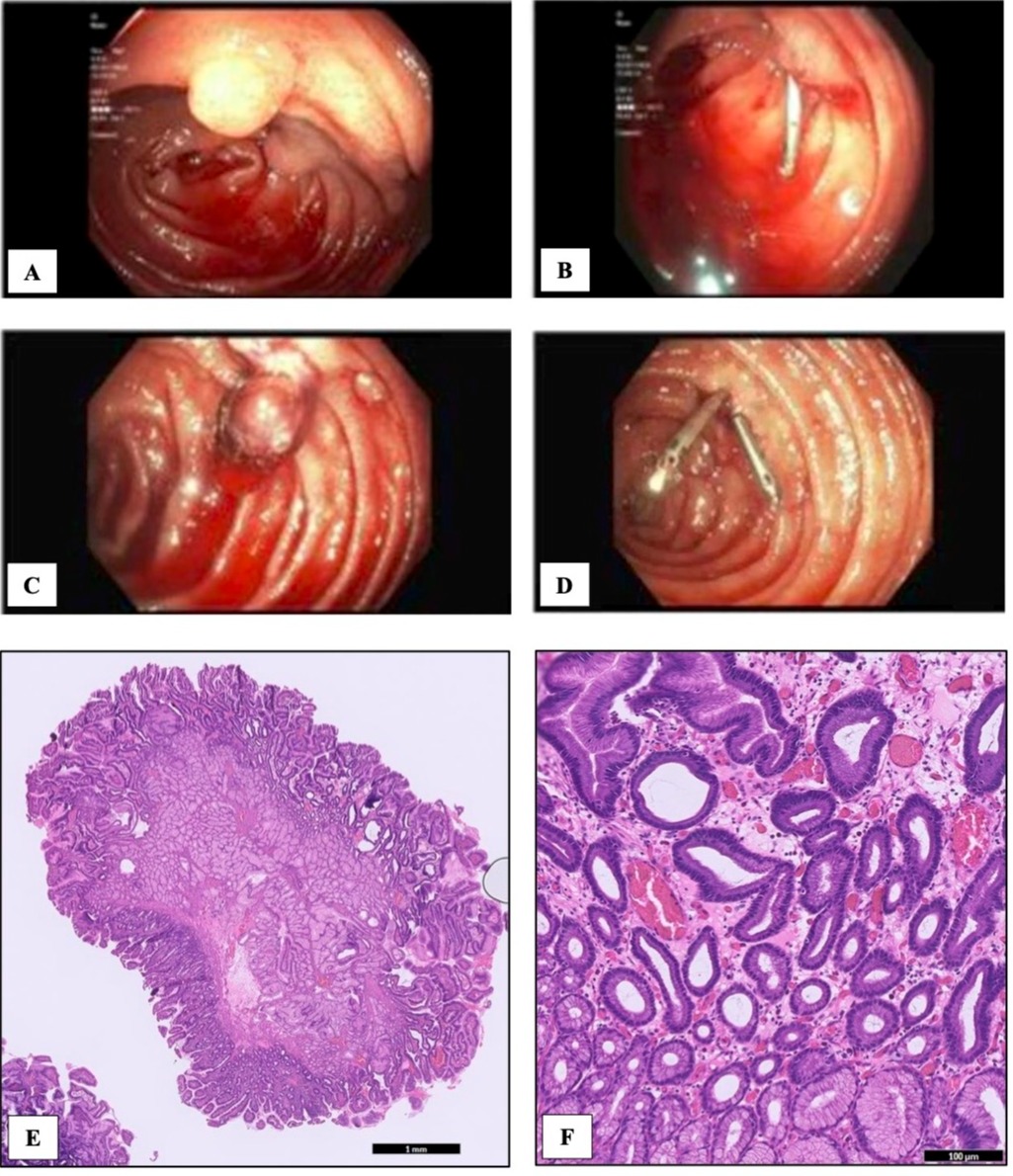
Case Description/Methods: A 58-year-old man with a history of ANCA vasculitis, heart transplant (on tacrolimus 10 mg BID and aspirin 81 mg QD), end-stage renal disease, hypertension, obesity, and obstructive sleep apnea presented with dizziness during dialysis 5 days after undergoing esophagogastroduodenoscopy (EGD) and colonoscopy for evaluation of diarrhea and unintentional weight loss. EGD revealed erythema in the duodenal bulb and D2, and two polyps in D3 (Image A). One 1 cm polyp was removed with hot polypectomy followed by endoclip and another with cold polypectomy (Image B). Patient reported same-day hematochezia followed by daily melena. On presentation 5 days after the EGD, vital signs were normal, but hemoglobin had dropped from 10.9 to 6 g/dl. Physical exam revealed conjunctival pallor. Repeat EGD showed two polypectomy sites – one with active oozing from under a large adherent clot (Image C). The large clot was removed and two endoclips were placed with subsequent hemostasis (Image D). Hemoglobin normalized following multiple transfusions. Pathology revealed a duodenal pyloric gland adenoma (Image E, F) and duodenal lymphangiectasia, respectively, as well as foveolar metaplasia in random duodenal biopsies.
Discussion: PGAs are most common in the stomach and are associated with atrophic autoimmune gastritis, H. pylori-associated gastritis, and found in older females. PGAs typically appear in a background of chronically inflamed mucosa. PGAs in the duodenum can occur in the setting of heterotopic gastric mucosa. Our presentation is rare due to the location of the PGA in the duodenum and atypical patient demographics (middle-aged male). The patient was on high-dose immunosuppression with a calcineurin inhibitor, which have been shown to increase the risk of malignancy after solid organ transplant. It is possible that this patient’s immunosuppression with tacrolimus increased the risk of developing a PGA in a background of foveolar metaplasia of the duodenum. Endoscopic surveillance at 1-6 months after initial procedure then every 3-12 months for ≥ 2 years is recommended for this patient with a duodenal PGA.
Disclosures:
Adrienne M. Bielawski, MD1, Amanda Rupert, MD2, Kuaybe Karakus Gulen, MD2, Frederick Yick, MD2. P3277 - Duodenal Pyloric Gland Adenoma in an Immunocompromised Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, NY; 2Westchester Medical Center, Valhalla, NY
Introduction: A pyloric gland adenoma (PGA) is a rare neoplasm that can present as a duodenal non-ampullary polyp. PGAs can progress to invasive adenocarcinoma and should undergo resection and surveillance, although recurrence is rare. We report a case of an upper gastrointestinal bleed following resection of a duodenal polyp later identified as a PGA in an immunocompromised patient.
Case Description/Methods: A 58-year-old man with a history of ANCA vasculitis, heart transplant (on tacrolimus 10 mg BID and aspirin 81 mg QD), end-stage renal disease, hypertension, obesity, and obstructive sleep apnea presented with dizziness during dialysis 5 days after undergoing esophagogastroduodenoscopy (EGD) and colonoscopy for evaluation of diarrhea and unintentional weight loss. EGD revealed erythema in the duodenal bulb and D2, and two polyps in D3 (Image A). One 1 cm polyp was removed with hot polypectomy followed by endoclip and another with cold polypectomy (Image B). Patient reported same-day hematochezia followed by daily melena. On presentation 5 days after the EGD, vital signs were normal, but hemoglobin had dropped from 10.9 to 6 g/dl. Physical exam revealed conjunctival pallor. Repeat EGD showed two polypectomy sites – one with active oozing from under a large adherent clot (Image C). The large clot was removed and two endoclips were placed with subsequent hemostasis (Image D). Hemoglobin normalized following multiple transfusions. Pathology revealed a duodenal pyloric gland adenoma (Image E, F) and duodenal lymphangiectasia, respectively, as well as foveolar metaplasia in random duodenal biopsies.
Discussion: PGAs are most common in the stomach and are associated with atrophic autoimmune gastritis, H. pylori-associated gastritis, and found in older females. PGAs typically appear in a background of chronically inflamed mucosa. PGAs in the duodenum can occur in the setting of heterotopic gastric mucosa. Our presentation is rare due to the location of the PGA in the duodenum and atypical patient demographics (middle-aged male). The patient was on high-dose immunosuppression with a calcineurin inhibitor, which have been shown to increase the risk of malignancy after solid organ transplant. It is possible that this patient’s immunosuppression with tacrolimus increased the risk of developing a PGA in a background of foveolar metaplasia of the duodenum. Endoscopic surveillance at 1-6 months after initial procedure then every 3-12 months for ≥ 2 years is recommended for this patient with a duodenal PGA.
Figure: Esophagogastroduodenoscopy (EGD) showing two duodenal polyps (A) followed by polypectomy site with endoclip (B); repeat EGD showing adherent clot and active bleeding from polypectomy site (C) followed by hemostasis with two endoclips (D); hematoxylin & eosin (H&E) stain of the pyloric gland adenoma (E); H&E stain revealing pyloric glands (F).
Disclosures:
Adrienne Bielawski indicated no relevant financial relationships.
Amanda Rupert indicated no relevant financial relationships.
Kuaybe Karakus Gulen indicated no relevant financial relationships.
Frederick Yick indicated no relevant financial relationships.
Adrienne M. Bielawski, MD1, Amanda Rupert, MD2, Kuaybe Karakus Gulen, MD2, Frederick Yick, MD2. P3277 - Duodenal Pyloric Gland Adenoma in an Immunocompromised Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
