Monday Poster Session
Category: Small Intestine
P3211 - The Experience of Bone Health Evaluation and Management Among Adult Patients with Celiac Disease at a Tertiary Center
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Kinan Obeidat, MD
University of Texas Medical Branch
Santa Fe, TX
Presenting Author(s)
Kinan Obeidat, MD1, Abdulla Massad, MD2, Minh Tran, MD2, Garrett T. Coleman, 3, Brooke Corning, MD2
1University of Texas Medical Branch, Santa Fe, TX; 2University of Texas Medical Branch, Galveston, TX; 3University of Texas Medical Branch, John Sealy School of Medicine, Galveston, TX
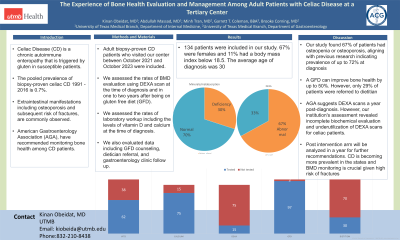
Introduction: Celiac Disease (CD) is a chronic autoimmune enteropathy that is triggered by exposure to gluten in genetically susceptible patients. The pooled global prevalence of biopsy-proven celiac disease from 1991 through 2016 is 0.7%. Diarrhea is the typical presentation, but extraintestinal manifestations including osteoporosis and subsequent risk of fractures, are commonly observed. Several guidelines, including the American Gastroenterology Association (AGA), have recommended monitoring bone health among CD patients. We sought to assess CD-related skeletal health at our institution.
Methods: Adult patients with biopsy-proven celiac disease who visited our center between October 2021 and October 2023 were included. Chart review was performed to assess the rates of BMD evaluation using DEXA scan at the time of diagnosis and in one to two years after being on gluten free diet (GFD). We assessed the rates of laboratory workup including the levels of vitamin D and calcium at the time of diagnosis. We also evaluated data including GFD counseling, dietician referral, and gastroenterology clinic follow up.
Results: 134 patients were included in our study. 67% were females and 11% had a body mass index below 18.5. The average age of diagnosis was 30, with over 70% aged between 18 and 50. 62% and 75% of patients obtained vitamin D and calcium levels respectively, with at least 30% having vitamin D deficiency or symptoms of malabsorption at the time of diagnosis. The frequency of patients who underwent DEXA scan at the time of diagnosis or in 1-2 years for surveillance was 15%. Among those, 67% of patients were found to have either osteopenia or osteoporosis. When seen in the clinic, 97% of patients were counseled on GFD adherence, and 29% were referred to a dietician.
Discussion: CD can cause BMD loss through immune and inflammatory changes, with studies indicating osteopenia or osteoporosis prevalence of up to 72% at diagnosis, correlating with higher fracture risk. Our study found 67% of patients with these conditions, aligning with previous research. A GFD, the primary treatment, can improve bone health by up to 50%. However, only 29% of patients were referred to dietitians despite AGA's recommendation for lifelong adherence and dietician involvement. Guidelines vary on BMD screening, with AGA suggesting DEXA scans a year post-diagnosis. However, our institution's assessment revealed shortcomings characterized by incomplete biochemical evaluation and underutilization of DEXA scans for celiac patients.
Disclosures:
Kinan Obeidat, MD1, Abdulla Massad, MD2, Minh Tran, MD2, Garrett T. Coleman, 3, Brooke Corning, MD2. P3211 - The Experience of Bone Health Evaluation and Management Among Adult Patients with Celiac Disease at a Tertiary Center, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Medical Branch, Santa Fe, TX; 2University of Texas Medical Branch, Galveston, TX; 3University of Texas Medical Branch, John Sealy School of Medicine, Galveston, TX
Introduction: Celiac Disease (CD) is a chronic autoimmune enteropathy that is triggered by exposure to gluten in genetically susceptible patients. The pooled global prevalence of biopsy-proven celiac disease from 1991 through 2016 is 0.7%. Diarrhea is the typical presentation, but extraintestinal manifestations including osteoporosis and subsequent risk of fractures, are commonly observed. Several guidelines, including the American Gastroenterology Association (AGA), have recommended monitoring bone health among CD patients. We sought to assess CD-related skeletal health at our institution.
Methods: Adult patients with biopsy-proven celiac disease who visited our center between October 2021 and October 2023 were included. Chart review was performed to assess the rates of BMD evaluation using DEXA scan at the time of diagnosis and in one to two years after being on gluten free diet (GFD). We assessed the rates of laboratory workup including the levels of vitamin D and calcium at the time of diagnosis. We also evaluated data including GFD counseling, dietician referral, and gastroenterology clinic follow up.
Results: 134 patients were included in our study. 67% were females and 11% had a body mass index below 18.5. The average age of diagnosis was 30, with over 70% aged between 18 and 50. 62% and 75% of patients obtained vitamin D and calcium levels respectively, with at least 30% having vitamin D deficiency or symptoms of malabsorption at the time of diagnosis. The frequency of patients who underwent DEXA scan at the time of diagnosis or in 1-2 years for surveillance was 15%. Among those, 67% of patients were found to have either osteopenia or osteoporosis. When seen in the clinic, 97% of patients were counseled on GFD adherence, and 29% were referred to a dietician.
Discussion: CD can cause BMD loss through immune and inflammatory changes, with studies indicating osteopenia or osteoporosis prevalence of up to 72% at diagnosis, correlating with higher fracture risk. Our study found 67% of patients with these conditions, aligning with previous research. A GFD, the primary treatment, can improve bone health by up to 50%. However, only 29% of patients were referred to dietitians despite AGA's recommendation for lifelong adherence and dietician involvement. Guidelines vary on BMD screening, with AGA suggesting DEXA scans a year post-diagnosis. However, our institution's assessment revealed shortcomings characterized by incomplete biochemical evaluation and underutilization of DEXA scans for celiac patients.
Disclosures:
Kinan Obeidat indicated no relevant financial relationships.
Abdulla Massad indicated no relevant financial relationships.
Minh Tran indicated no relevant financial relationships.
Garrett Coleman indicated no relevant financial relationships.
Brooke Corning indicated no relevant financial relationships.
Kinan Obeidat, MD1, Abdulla Massad, MD2, Minh Tran, MD2, Garrett T. Coleman, 3, Brooke Corning, MD2. P3211 - The Experience of Bone Health Evaluation and Management Among Adult Patients with Celiac Disease at a Tertiary Center, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
