Monday Poster Session
Category: Small Intestine
P3219 - Complications of IPEX Syndrome with Crohn’s-Like Enterocolonopathy Resulting in Short Gut Syndrome
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Abdullah A. Memon, MD
University of Illinois College of Medicine
Chicago, IL
Presenting Author(s)
Abdullah Memon, MD1, Dexter Nwachukwu, MD2, Omar T. Ahmed, MD2, Robert E.. Carroll, MD2
1University of Illinois College of Medicine, Chicago, IL; 2University of Illinois at Chicago, Chicago, IL
Introduction: Immune dysregulation, polyendocrinopathy, enteropathy, X-lined (IPEX) syndrome is caused by mutations in the FOXP3 gene, a transcriptional regulator required for regulatory T cells. IPEX syndrome typically presents with diabetes, failure to thrive, eczema, and hypo- or hyperthyroidism. The predominant clinical feature is an autoimmune enteropathy with watery diarrhea that may mimic inflammatory bowel disease (IBD). We present a case of a patient with IPEX syndrome resulting in Crohn’s-like IBD with a complicated abdominal surgical history, resulting in short gut syndrome.
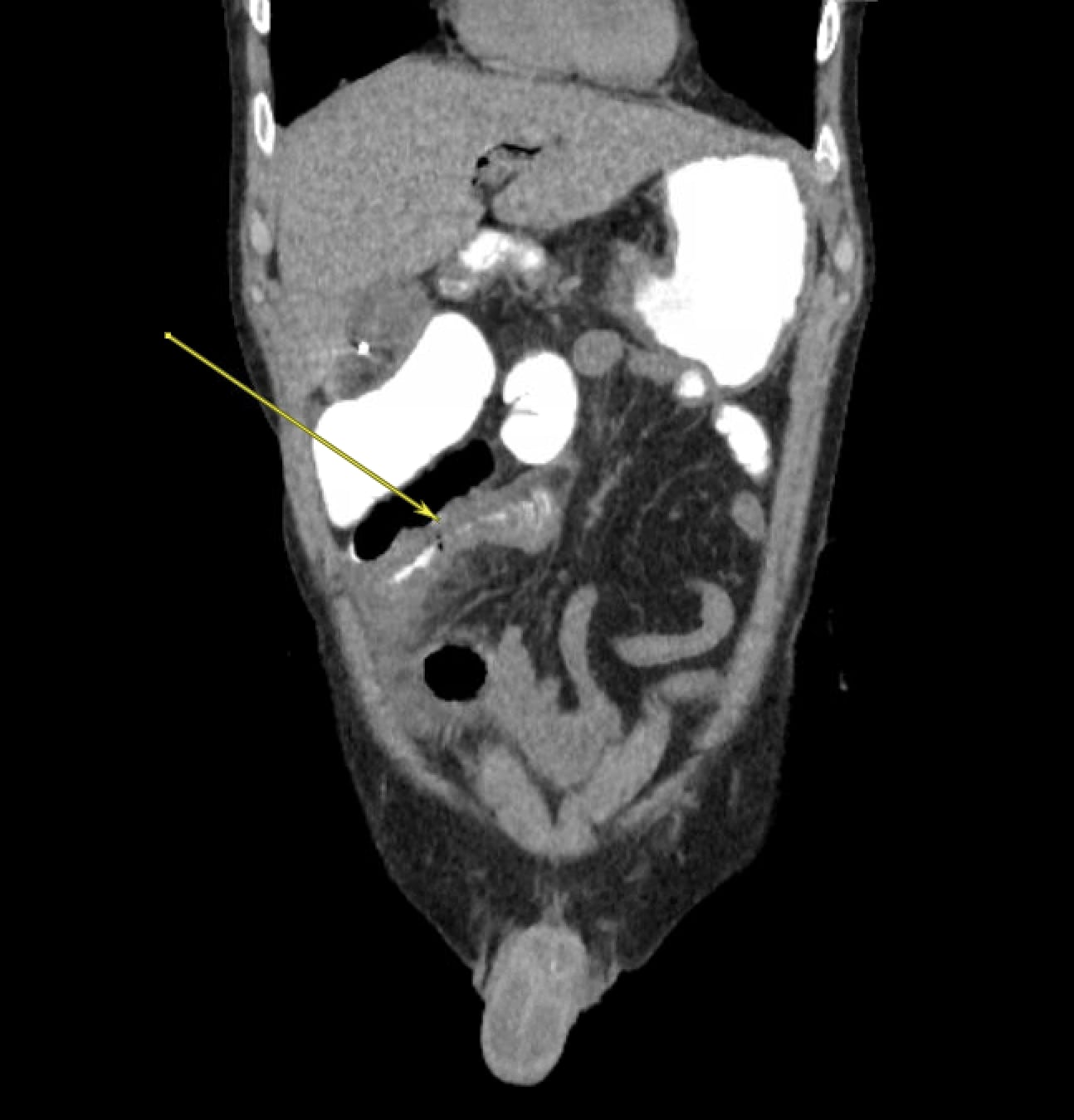
Case Description/Methods: A 27 year-old male with past medical history significant for IPEX syndrome with Crohn’s like enterocolonopathy presented with acute on chronic abdominal pain, vomiting, and decreased stool output. His GI history was complex, as he had a partial proctocolectomy at age 6 with subsequent J pouch creation at age 13. He had an end-ileostomy after a failed ileoanal pouch due to chronic pouchitis at age 18, complicated by high output ileostomy and fistula, ostomy stenosis and prolapse, bleeding from ostomy requiring chronic IV fluid replacement and TPN, as well as frequent partial small bowel obstructions (SBOs). Prior to admission, he wanted to establish care at our institution for small bowel transplant and/or fistula repair. Labs were at baseline, and CT abdomen/pelvis showed mildly dilated contrast-filled small bowel loops in the right hemiabdomen with transition point proximal to the midline ileostomy, possibly suggesting ileus versus SBO. His symptoms improved with bowel rest and IV fluids, and he was discharged with teduglutide and outpatient follow up with GI and general surgery.
Discussion: IPEX syndrome most commmonly manifests as an autoimmune enteropathy, which may be similar to Crohn’s disease, as it presents with watery diarrhea and has histology notable for lymphocytic infiltration in the lamina propria. Failure to thrive can follow, with many patients requiring TPN. Immunosuppression can also be used to manage the diarrhea. Our patient was TPN-dependent for over 3 years and on tacrolimus at the time of presentation. Nevertheless, this IBD-like enterocolonopathy can lead to complications, requiring abdominal surgeries and resulting in short gut syndrome, for which treatment should be directed towards, as in our case. A multidisciplinary team of surgery, gastroenterology, and nutrition should be closely following these patients to prevent potentially severe complications of short gut syndrome.
Disclosures:
Abdullah Memon, MD1, Dexter Nwachukwu, MD2, Omar T. Ahmed, MD2, Robert E.. Carroll, MD2. P3219 - Complications of IPEX Syndrome with Crohn’s-Like Enterocolonopathy Resulting in Short Gut Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Illinois College of Medicine, Chicago, IL; 2University of Illinois at Chicago, Chicago, IL
Introduction: Immune dysregulation, polyendocrinopathy, enteropathy, X-lined (IPEX) syndrome is caused by mutations in the FOXP3 gene, a transcriptional regulator required for regulatory T cells. IPEX syndrome typically presents with diabetes, failure to thrive, eczema, and hypo- or hyperthyroidism. The predominant clinical feature is an autoimmune enteropathy with watery diarrhea that may mimic inflammatory bowel disease (IBD). We present a case of a patient with IPEX syndrome resulting in Crohn’s-like IBD with a complicated abdominal surgical history, resulting in short gut syndrome.
Case Description/Methods: A 27 year-old male with past medical history significant for IPEX syndrome with Crohn’s like enterocolonopathy presented with acute on chronic abdominal pain, vomiting, and decreased stool output. His GI history was complex, as he had a partial proctocolectomy at age 6 with subsequent J pouch creation at age 13. He had an end-ileostomy after a failed ileoanal pouch due to chronic pouchitis at age 18, complicated by high output ileostomy and fistula, ostomy stenosis and prolapse, bleeding from ostomy requiring chronic IV fluid replacement and TPN, as well as frequent partial small bowel obstructions (SBOs). Prior to admission, he wanted to establish care at our institution for small bowel transplant and/or fistula repair. Labs were at baseline, and CT abdomen/pelvis showed mildly dilated contrast-filled small bowel loops in the right hemiabdomen with transition point proximal to the midline ileostomy, possibly suggesting ileus versus SBO. His symptoms improved with bowel rest and IV fluids, and he was discharged with teduglutide and outpatient follow up with GI and general surgery.
Discussion: IPEX syndrome most commmonly manifests as an autoimmune enteropathy, which may be similar to Crohn’s disease, as it presents with watery diarrhea and has histology notable for lymphocytic infiltration in the lamina propria. Failure to thrive can follow, with many patients requiring TPN. Immunosuppression can also be used to manage the diarrhea. Our patient was TPN-dependent for over 3 years and on tacrolimus at the time of presentation. Nevertheless, this IBD-like enterocolonopathy can lead to complications, requiring abdominal surgeries and resulting in short gut syndrome, for which treatment should be directed towards, as in our case. A multidisciplinary team of surgery, gastroenterology, and nutrition should be closely following these patients to prevent potentially severe complications of short gut syndrome.
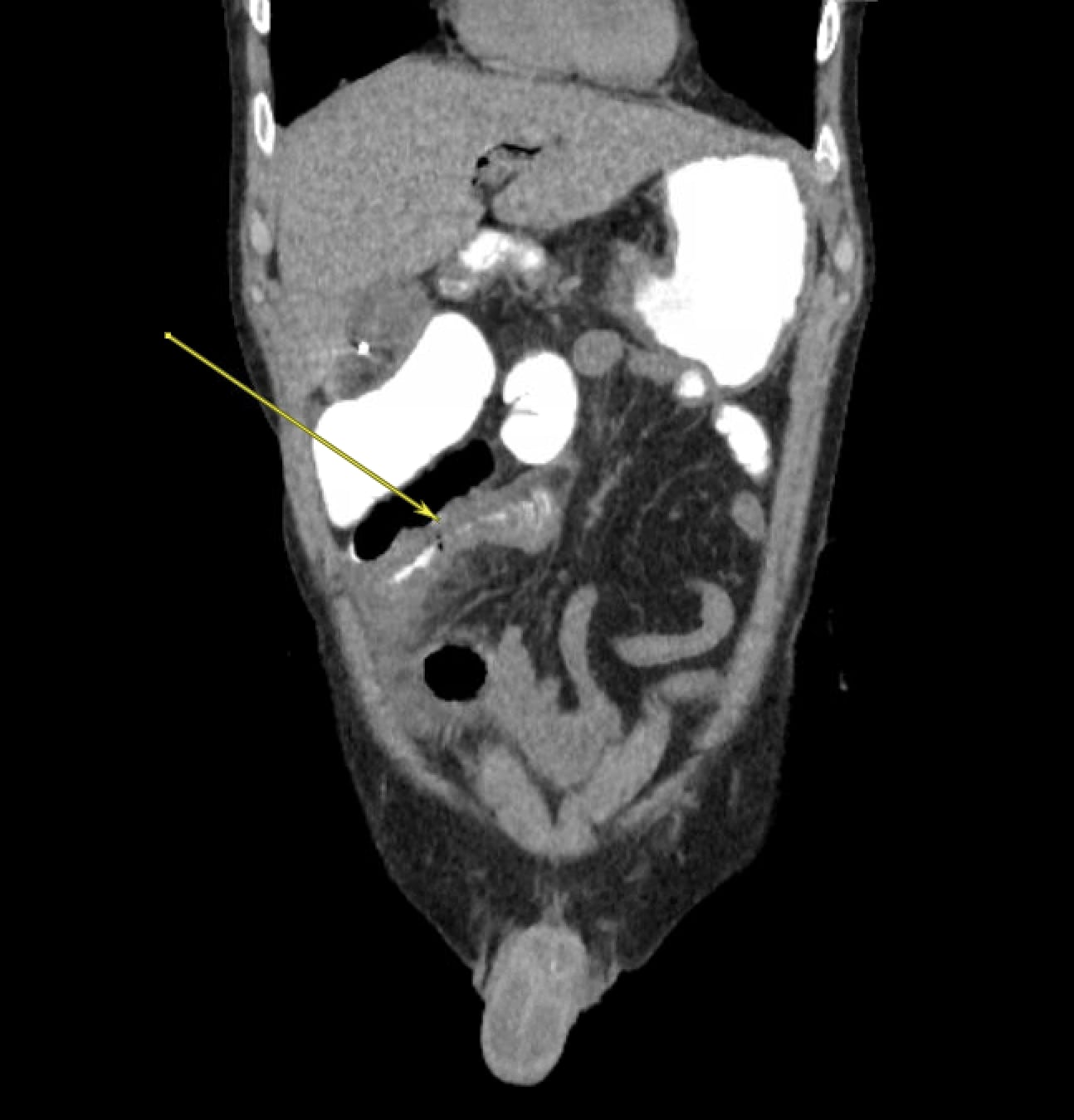
Figure: Transition point seen proximal to the midline ileostomy, suggesting possible ileus versus SBO.
Disclosures:
Abdullah Memon indicated no relevant financial relationships.
Dexter Nwachukwu indicated no relevant financial relationships.
Omar Ahmed indicated no relevant financial relationships.
Robert Carroll indicated no relevant financial relationships.
Abdullah Memon, MD1, Dexter Nwachukwu, MD2, Omar T. Ahmed, MD2, Robert E.. Carroll, MD2. P3219 - Complications of IPEX Syndrome with Crohn’s-Like Enterocolonopathy Resulting in Short Gut Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
