Monday Poster Session
Category: Small Intestine
P3221 - Navigating Therapeutic Challenges: Recurrent Gastrointestinal Bleeding in Klippel-Trenaunay Syndrome
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Isabella Suarez Alcala, MD
Palmetto General Hospital
Hialeah, FL
Presenting Author(s)
Isabella Suarez Alcala, MD1, Natasha Mederos, MD2, Akram Ahmad, MD3, Jacob Ukleja, MS4, Andrew Ukleja, MD3
1Palmetto General Hospital, Hialeah, FL; 2University of Miami Miller School of Medicine at Holy Cross Hospital, Fort Lauderdale, FL; 3Cleveland Clinic Florida, Weston, FL; 4University of Central Florida College of Medicine, Orlando, FL
Introduction: Klippel-Trenaunay Syndrome (KTS) is a rare congenital disorder commonly associated with the PIK3CA gene mutation, which increases cell proliferation. KTS is characterized by venous, capillary malformations, and limb overgrowth, occasionally accompanied by lymphatic abnormalities. Gastrointestinal (GI) bleeding in patients with KTS is a challenging complication. We report the case of a patient with KTS who underwent multiple bowel resections to manage recurrent GI bleeding.
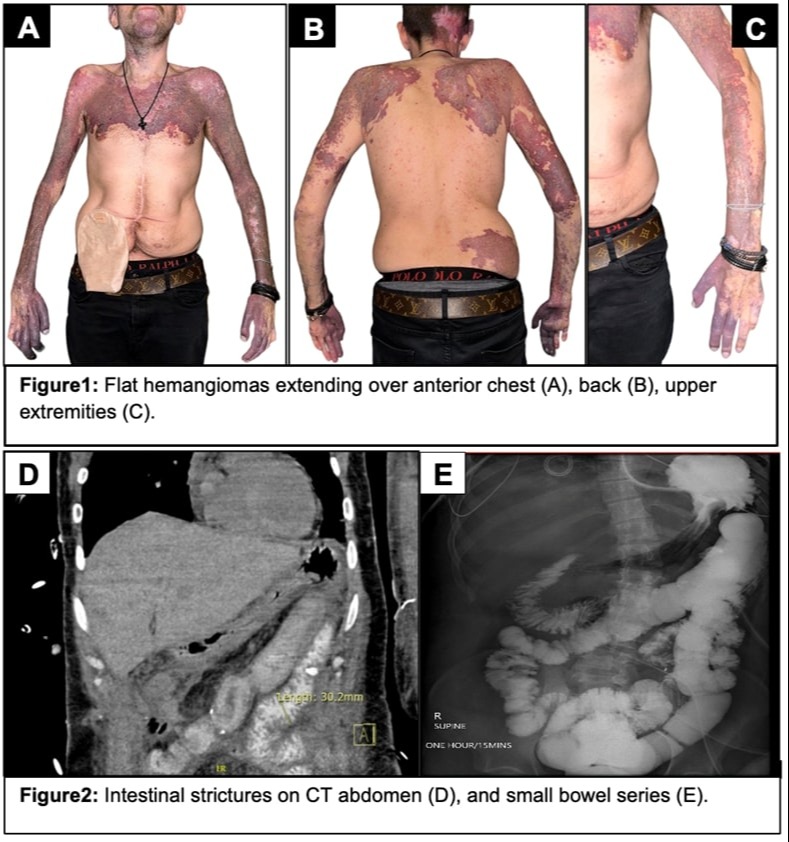
Case Description/Methods: A 33-year-old male with KTS presented with persistent GI bleeding despite prior intestinal resections. He was born with hemangiomas in his face, upper extremities, upper chest, and back (Fig. 1). He experienced frequent GI bleeds during his infancy. Because of major GI bleeding at age 23, he underwent GI work up including EGD, colonoscopy, CT enterography, and capsule endoscopy with findings of congestive enteropathy, gastric, small bowel, and colonic varices, and AVMs. At that time embolization of the distal jejunal artery branches was performed. Another major GI bleed at age 24 resulted in cardiac arrest due to hemorrhagic shock, prompting an emergent hemicolectomy and partial small bowel resection. Seven years later, further small bowel resections were complicated by anastomotic dehiscence, resulting in an ileostomy. Because of recurrent GI bleeding, he was evaluated at an outside transplant center but declined an intestinal transplant, opting for conservative medical management with propranolol and estrogen. Subsequently, he sought a second opinion at our center due to ongoing stoma bleeding refractory to medical therapy. Double balloon enteroscopy and ileoscopy revealed large, non-bleeding varices and AVMs requiring small bowel resection, lysis of adhesions, and ileostomy reversal, followed by intestinal anastomosis, gastro-duodenal varices ligature, and abdominal wall closure. Currently, he remains hospitalized with no new bleeding episodes since the surgery. He requires parenteral support due to SBS with total small bowel length of 150 cm.
Discussion: Managing GI bleeding in KTS is complicated by the inherent vascular anomalies, requiring a multidisciplinary approach. Despite multiple surgical and interventional radiology attempts to control bleeding, the patient's quality of life remains significantly impaired, illustrating the challenges in managing KTS. This case advocates for further research into genetic underpinnings and new medical therapies that may help such patients.
Disclosures:
Isabella Suarez Alcala, MD1, Natasha Mederos, MD2, Akram Ahmad, MD3, Jacob Ukleja, MS4, Andrew Ukleja, MD3. P3221 - Navigating Therapeutic Challenges: Recurrent Gastrointestinal Bleeding in Klippel-Trenaunay Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Palmetto General Hospital, Hialeah, FL; 2University of Miami Miller School of Medicine at Holy Cross Hospital, Fort Lauderdale, FL; 3Cleveland Clinic Florida, Weston, FL; 4University of Central Florida College of Medicine, Orlando, FL
Introduction: Klippel-Trenaunay Syndrome (KTS) is a rare congenital disorder commonly associated with the PIK3CA gene mutation, which increases cell proliferation. KTS is characterized by venous, capillary malformations, and limb overgrowth, occasionally accompanied by lymphatic abnormalities. Gastrointestinal (GI) bleeding in patients with KTS is a challenging complication. We report the case of a patient with KTS who underwent multiple bowel resections to manage recurrent GI bleeding.
Case Description/Methods: A 33-year-old male with KTS presented with persistent GI bleeding despite prior intestinal resections. He was born with hemangiomas in his face, upper extremities, upper chest, and back (Fig. 1). He experienced frequent GI bleeds during his infancy. Because of major GI bleeding at age 23, he underwent GI work up including EGD, colonoscopy, CT enterography, and capsule endoscopy with findings of congestive enteropathy, gastric, small bowel, and colonic varices, and AVMs. At that time embolization of the distal jejunal artery branches was performed. Another major GI bleed at age 24 resulted in cardiac arrest due to hemorrhagic shock, prompting an emergent hemicolectomy and partial small bowel resection. Seven years later, further small bowel resections were complicated by anastomotic dehiscence, resulting in an ileostomy. Because of recurrent GI bleeding, he was evaluated at an outside transplant center but declined an intestinal transplant, opting for conservative medical management with propranolol and estrogen. Subsequently, he sought a second opinion at our center due to ongoing stoma bleeding refractory to medical therapy. Double balloon enteroscopy and ileoscopy revealed large, non-bleeding varices and AVMs requiring small bowel resection, lysis of adhesions, and ileostomy reversal, followed by intestinal anastomosis, gastro-duodenal varices ligature, and abdominal wall closure. Currently, he remains hospitalized with no new bleeding episodes since the surgery. He requires parenteral support due to SBS with total small bowel length of 150 cm.
Discussion: Managing GI bleeding in KTS is complicated by the inherent vascular anomalies, requiring a multidisciplinary approach. Despite multiple surgical and interventional radiology attempts to control bleeding, the patient's quality of life remains significantly impaired, illustrating the challenges in managing KTS. This case advocates for further research into genetic underpinnings and new medical therapies that may help such patients.
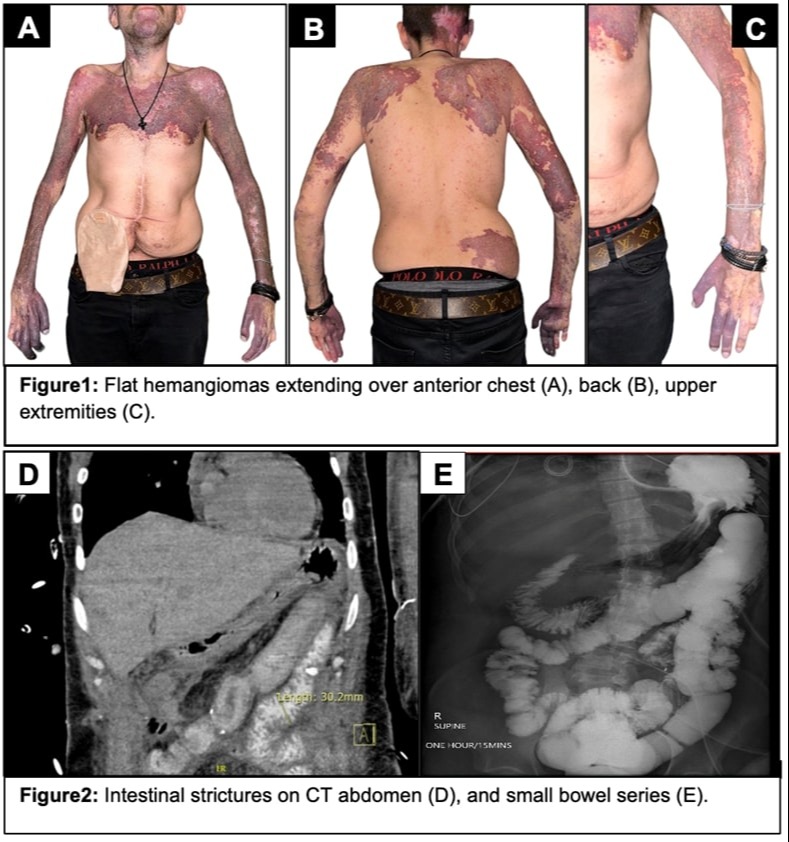
Figure: Figure 1
Disclosures:
Isabella Suarez Alcala indicated no relevant financial relationships.
Natasha Mederos indicated no relevant financial relationships.
Akram Ahmad indicated no relevant financial relationships.
Jacob Ukleja indicated no relevant financial relationships.
Andrew Ukleja indicated no relevant financial relationships.
Isabella Suarez Alcala, MD1, Natasha Mederos, MD2, Akram Ahmad, MD3, Jacob Ukleja, MS4, Andrew Ukleja, MD3. P3221 - Navigating Therapeutic Challenges: Recurrent Gastrointestinal Bleeding in Klippel-Trenaunay Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
