Monday Poster Session
Category: Small Intestine
P3226 - Bilateral Adrenal Hemorrhage Unveiling Acute Mesenteric Ischemia: A Comprehensive Case Report
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Sagar Nagpal, MD
East Tennessee State University Quillen College of Medicine
Johnson City, TN
Presenting Author(s)
Sagar Nagpal, MD1, Hezborn Magacha, MD, MPH1, Pooja Bhandari, MD2, Davis Berry, DO1, Arwa Zakaria, DO1, Chakradhar Reddy, MD1
1East Tennessee State University Quillen College of Medicine, Johnson City, TN; 2University of Mississippi Medical Center, Jackson, MS
Introduction: Acute mesenteric ischemia is a multifaceted condition involving diverse disorders impacting blood flow to the abdominal viscera, with reported incidences ranging between 5.3 and 8.4 cases per 100,000 per year. The associated mortality for mesenteric ischemia varies widely, from 30% to 90%. Conversely, adrenal hemorrhage, often linked to stress, trauma, or coagulopathy, can lead to adrenal crisis and potential shock.
Case Description/Methods: A 52-year-old male, chronically ill with a significant medical history including EtOH dependence, chronic obstructive pulmonary disease (COPD), and coronary artery disease was admitted after being discovered by a friend lying on the floor, confused, and covered in urine and feces. The patient presented with hypothermia, hypotension, and laboratory abnormalities indicative of acute kidney injury (AKI). He was admitted for further evaluation of suspected septic shock. Following broad-spectrum antibiotics and fluid administration, the patient's condition improved.
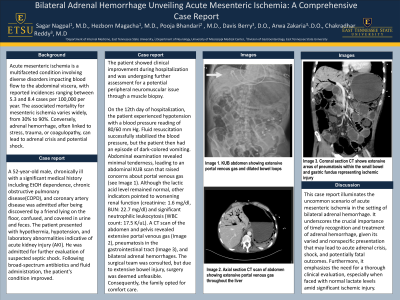
On the 12th day of hospitalization, the patient experienced hypotension with a blood pressure reading of 80/60 mm Hg. Fluid resuscitation successfully stabilized the blood pressure, but the patient then had an episode of dark-colored vomiting. Abdominal examination revealed minimal tenderness, leading to an abdominal KUB scan that raised concerns about portal venous gas (see Image 1). Although the lactic acid level remained normal, other indicators pointed to worsening renal function (creatinine: 1.6 mg/dl, BUN: 22.7 mg/dl) and significant neutrophilic leukocytosis (WBC count: 17.5 K/uL). A CT scan of the abdomen and pelvis revealed extensive portal venous gas (Image 2), pneumatosis in the gastrointestinal tract (Image 3), and bilateral adrenal hemorrhages. The surgical team was consulted, but due to extensive bowel injury, surgery was deemed unfeasible. Consequently, the family opted for comfort care.
Discussion: This case report illuminates the uncommon scenario of acute mesenteric ischemia in the setting of bilateral adrenal hemorrhage. It underscores the crucial importance of timely recognition and treatment of adrenal hemorrhage, given its varied and nonspecific presentation that may lead to acute adrenal crisis, shock, and potentially fatal outcomes. Furthermore, it emphasizes the need for a thorough clinical evaluation, especially when faced with normal lactate levels amid significant ischemic injury.

Disclosures:
Sagar Nagpal, MD1, Hezborn Magacha, MD, MPH1, Pooja Bhandari, MD2, Davis Berry, DO1, Arwa Zakaria, DO1, Chakradhar Reddy, MD1. P3226 - Bilateral Adrenal Hemorrhage Unveiling Acute Mesenteric Ischemia: A Comprehensive Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1East Tennessee State University Quillen College of Medicine, Johnson City, TN; 2University of Mississippi Medical Center, Jackson, MS
Introduction: Acute mesenteric ischemia is a multifaceted condition involving diverse disorders impacting blood flow to the abdominal viscera, with reported incidences ranging between 5.3 and 8.4 cases per 100,000 per year. The associated mortality for mesenteric ischemia varies widely, from 30% to 90%. Conversely, adrenal hemorrhage, often linked to stress, trauma, or coagulopathy, can lead to adrenal crisis and potential shock.
Case Description/Methods: A 52-year-old male, chronically ill with a significant medical history including EtOH dependence, chronic obstructive pulmonary disease (COPD), and coronary artery disease was admitted after being discovered by a friend lying on the floor, confused, and covered in urine and feces. The patient presented with hypothermia, hypotension, and laboratory abnormalities indicative of acute kidney injury (AKI). He was admitted for further evaluation of suspected septic shock. Following broad-spectrum antibiotics and fluid administration, the patient's condition improved.
On the 12th day of hospitalization, the patient experienced hypotension with a blood pressure reading of 80/60 mm Hg. Fluid resuscitation successfully stabilized the blood pressure, but the patient then had an episode of dark-colored vomiting. Abdominal examination revealed minimal tenderness, leading to an abdominal KUB scan that raised concerns about portal venous gas (see Image 1). Although the lactic acid level remained normal, other indicators pointed to worsening renal function (creatinine: 1.6 mg/dl, BUN: 22.7 mg/dl) and significant neutrophilic leukocytosis (WBC count: 17.5 K/uL). A CT scan of the abdomen and pelvis revealed extensive portal venous gas (Image 2), pneumatosis in the gastrointestinal tract (Image 3), and bilateral adrenal hemorrhages. The surgical team was consulted, but due to extensive bowel injury, surgery was deemed unfeasible. Consequently, the family opted for comfort care.
Discussion: This case report illuminates the uncommon scenario of acute mesenteric ischemia in the setting of bilateral adrenal hemorrhage. It underscores the crucial importance of timely recognition and treatment of adrenal hemorrhage, given its varied and nonspecific presentation that may lead to acute adrenal crisis, shock, and potentially fatal outcomes. Furthermore, it emphasizes the need for a thorough clinical evaluation, especially when faced with normal lactate levels amid significant ischemic injury.

Figure: Coronal section CT shows extensive areas of pneumatosis within the small bowel and gastric fundus representing ischemic injury
Disclosures:
Sagar Nagpal indicated no relevant financial relationships.
Hezborn Magacha indicated no relevant financial relationships.
Pooja Bhandari indicated no relevant financial relationships.
Davis Berry indicated no relevant financial relationships.
Arwa Zakaria indicated no relevant financial relationships.
Chakradhar Reddy indicated no relevant financial relationships.
Sagar Nagpal, MD1, Hezborn Magacha, MD, MPH1, Pooja Bhandari, MD2, Davis Berry, DO1, Arwa Zakaria, DO1, Chakradhar Reddy, MD1. P3226 - Bilateral Adrenal Hemorrhage Unveiling Acute Mesenteric Ischemia: A Comprehensive Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
