Monday Poster Session
Category: Obesity
P3158 - Endoscopic Sleeve Gastroplasty Improves Atherosclerotic Cardiovascular Disease Risk Factors and Pooled Cohort Equations Risk Score: A Prospective Cohort Study
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ali Lahooti, BS
Weill Cornell Medicine
New York, NY
Presenting Author(s)
Award: Presidential Poster Award
Ali Lahooti, BS1, Anam Rizvi, MD1, Kate E. Johnson, BS1, Muhammad Usman. Baig, MBBS1, Cynthia Akagbosu, MD, MA1, SriHari Mahadev, MD2, Kartik Sampath, MD1, David L. Carr-Locke, MA, MD, FACG1, Alpana Shukla, MD1, Louis Aronne, MD1, Carolyn Newberry, MD2, Sonal Kumar, MD, MPH3, Reem Sharaiha, MD1
1Weill Cornell Medicine, New York, NY; 2New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 3Weill Cornell Medical College, New York, NY
Introduction: Endoscopic sleeve gastroplasty (ESG) is a novel, minimally invasive endobariatric technique that restricts the stomach's size to induce weight loss. We performed a prospective study to evaluate the reductions on the American College of Cardiology and the American Heart Association predicted atherosclerotic cardiovascular disease (ASCVD) risk and pharmacotherapy utilization 12 months after ESG.
Methods: Data was extracted from 404 consecutive patients undergoing ESG from August 2013 through June 2024. Inclusion criteria for the study were as follows: had a body mass index (BMI) exceeding 30 kg/m² (or >27 with comorbidities) and had not succeeded with non-surgical weight loss methods or had a BMI greater than 40 kg/m² and were either deemed unsuitable for surgical intervention or had declined surgery. Participants included in the ASCVD risk score analysis were aged 40 to 79 years. A single endoscopy specialist conducted all procedures by plicating the greater curvature of the stomach. Patients were evaluated after 12 months for anthropometric features (BMI, weight, blood pressure) and underwent metabolic serum tests. The primary outcomes were the effects of ESG on ASCVD risk score. Secondary outcomes were changes in medication usage and metabolic markers after ESG.
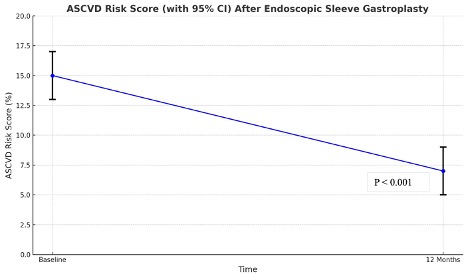
Results: 277 patients (7.5% female), (43% white) with a mean age of 51.4 ± 8.1 years, and mean BMI of 37.3±5.9 kg/m2 (27.1-64) underwent ESG and met inclusion criteria to have ASCVD risk evaluated. Meant total body weight loss TBWL at 1 year was 12.6% ±8.1. The patients’ mean ASCVD risk score was 8.1% at baseline, which was significantly reduced to 5.9% at 12 months (P < 0.001) (Figure 1). This reduction indicates a shift from intermediate to low risk of cardiovascular events over the next 10 years, even when accounting for the age-related increase in ASCVD scores. Additionally, there was a statistically significant decrease in the number of patients on antihypertensive (P < 0.001) and statin medications (P < 0.001) one-year post-procedure. There were significant reductions in metabolic and anthropometric markers seen one year post-ESG (Table 1).
Discussion: ESG is a minimally invasive endoscopic procedure that effectively promotes weight loss and improves cardiovascular risk factors in obese patients after one year. Additionally, there was significant reduction in the number of patients utilizing antihypertensives and statins. Further research is needed to evaluate the long-term impact of ESG on cardiovascular outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ali Lahooti, BS1, Anam Rizvi, MD1, Kate E. Johnson, BS1, Muhammad Usman. Baig, MBBS1, Cynthia Akagbosu, MD, MA1, SriHari Mahadev, MD2, Kartik Sampath, MD1, David L. Carr-Locke, MA, MD, FACG1, Alpana Shukla, MD1, Louis Aronne, MD1, Carolyn Newberry, MD2, Sonal Kumar, MD, MPH3, Reem Sharaiha, MD1. P3158 - Endoscopic Sleeve Gastroplasty Improves Atherosclerotic Cardiovascular Disease Risk Factors and Pooled Cohort Equations Risk Score: A Prospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Ali Lahooti, BS1, Anam Rizvi, MD1, Kate E. Johnson, BS1, Muhammad Usman. Baig, MBBS1, Cynthia Akagbosu, MD, MA1, SriHari Mahadev, MD2, Kartik Sampath, MD1, David L. Carr-Locke, MA, MD, FACG1, Alpana Shukla, MD1, Louis Aronne, MD1, Carolyn Newberry, MD2, Sonal Kumar, MD, MPH3, Reem Sharaiha, MD1
1Weill Cornell Medicine, New York, NY; 2New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 3Weill Cornell Medical College, New York, NY
Introduction: Endoscopic sleeve gastroplasty (ESG) is a novel, minimally invasive endobariatric technique that restricts the stomach's size to induce weight loss. We performed a prospective study to evaluate the reductions on the American College of Cardiology and the American Heart Association predicted atherosclerotic cardiovascular disease (ASCVD) risk and pharmacotherapy utilization 12 months after ESG.
Methods: Data was extracted from 404 consecutive patients undergoing ESG from August 2013 through June 2024. Inclusion criteria for the study were as follows: had a body mass index (BMI) exceeding 30 kg/m² (or >27 with comorbidities) and had not succeeded with non-surgical weight loss methods or had a BMI greater than 40 kg/m² and were either deemed unsuitable for surgical intervention or had declined surgery. Participants included in the ASCVD risk score analysis were aged 40 to 79 years. A single endoscopy specialist conducted all procedures by plicating the greater curvature of the stomach. Patients were evaluated after 12 months for anthropometric features (BMI, weight, blood pressure) and underwent metabolic serum tests. The primary outcomes were the effects of ESG on ASCVD risk score. Secondary outcomes were changes in medication usage and metabolic markers after ESG.
Results: 277 patients (7.5% female), (43% white) with a mean age of 51.4 ± 8.1 years, and mean BMI of 37.3±5.9 kg/m2 (27.1-64) underwent ESG and met inclusion criteria to have ASCVD risk evaluated. Meant total body weight loss TBWL at 1 year was 12.6% ±8.1. The patients’ mean ASCVD risk score was 8.1% at baseline, which was significantly reduced to 5.9% at 12 months (P < 0.001) (Figure 1). This reduction indicates a shift from intermediate to low risk of cardiovascular events over the next 10 years, even when accounting for the age-related increase in ASCVD scores. Additionally, there was a statistically significant decrease in the number of patients on antihypertensive (P < 0.001) and statin medications (P < 0.001) one-year post-procedure. There were significant reductions in metabolic and anthropometric markers seen one year post-ESG (Table 1).
Discussion: ESG is a minimally invasive endoscopic procedure that effectively promotes weight loss and improves cardiovascular risk factors in obese patients after one year. Additionally, there was significant reduction in the number of patients utilizing antihypertensives and statins. Further research is needed to evaluate the long-term impact of ESG on cardiovascular outcomes.
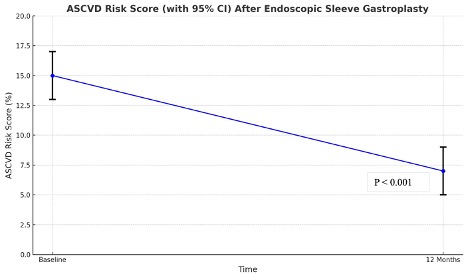
Figure: ASCVD risk score (with 95% CI) after endoscopic sleeve gastroplasty.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ali Lahooti indicated no relevant financial relationships.
Anam Rizvi indicated no relevant financial relationships.
Kate Johnson indicated no relevant financial relationships.
Muhammad Baig indicated no relevant financial relationships.
Cynthia Akagbosu indicated no relevant financial relationships.
SriHari Mahadev: Boston Scientific – Consultant. Conmed – Consultant.
Kartik Sampath indicated no relevant financial relationships.
David Carr-Locke: Steris Corporation – Royalties.
Alpana Shukla indicated no relevant financial relationships.
Louis Aronne: BMIQ – Advisory Committee/Board Member.
Carolyn Newberry: Nestle Nutrition Institute – Consultant.
Sonal Kumar: Intercept Pharmaceuticals, Inc. – Advisory Committee/Board Member, Speaker and site PI.
Reem Sharaiha: Boston Scientific – Consultant, Grant/Research Support. Olympus – Consultant. Surgical Intuitive – Advisory Committee/Board Member.
Ali Lahooti, BS1, Anam Rizvi, MD1, Kate E. Johnson, BS1, Muhammad Usman. Baig, MBBS1, Cynthia Akagbosu, MD, MA1, SriHari Mahadev, MD2, Kartik Sampath, MD1, David L. Carr-Locke, MA, MD, FACG1, Alpana Shukla, MD1, Louis Aronne, MD1, Carolyn Newberry, MD2, Sonal Kumar, MD, MPH3, Reem Sharaiha, MD1. P3158 - Endoscopic Sleeve Gastroplasty Improves Atherosclerotic Cardiovascular Disease Risk Factors and Pooled Cohort Equations Risk Score: A Prospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

