Monday Poster Session
Category: Liver
P3089 - An Intriguing Case of Direct Hyperbilirubinemia After Implantation of Left Ventricular Assist Device
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- PR
Pranav S. Ramamurthy, MD
University of Massachusetts Chan Medical School - Baystate Medical Center
Springfield, MA
Presenting Author(s)
Pranav S. Ramamurthy, MD1, Victoria A. Caruso, DO2, Omar Haider, MD1, Jacob Alexander, MD, DM3
1University of Massachusetts Chan Medical School - Baystate Medical Center, Springfield, MA; 2University of Massachusetts Chan Medical School - Baystate Medical Center, Windsor, CT; 3Baystate Medical Center, Springfield, MA
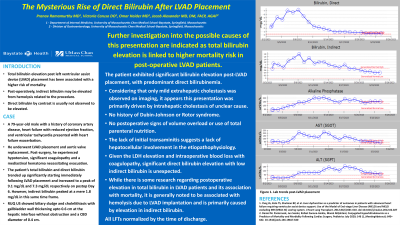
Introduction: Hyperbilirubinemia is well described after cardiac surgeries including implantation of left ventricular assist devices (LVAD) and has been found to be predictive of increased risk of morbidity and mortality. While intravascular hemolysis secondary to LVAD is often the primary mechanism for hyperbilirubinemia, we present a case that highlights the multifactorial origin of hyperbilirubinemia in this clinical situation.
Case Description/Methods: A 79-year-old male with a history of ischemic cardiomyopathy and aortic stenosis who was admitted with acute decompensated heart failure underwent implantation of LVAD and aortic valve replacement with bioprosthetic valve. The postoperative course was complicated by hypotension, coagulopathy and a mediastinal hematoma necessitating evacuation. He also required mechanical ventilation and multiple vasopressors which were eventually weaned off. His hemoglobin dropped to 7.8 g/dL post-operatively but recovered to 9.1 g/dL after transfusions. Electrolytes and creatinine remained normal. Lactate dehydrogenase peaked at 583 U/L. Liver function tests (LFTs) showed increasing total and direct bilirubin, peaking at 9.1 mg/dL and 7.3 mg/dL, respectively. Aspartate transaminase peaked at 215 U/L, alanine transaminase at 156 U/L and alkaline phosphatase at 204 U/L, three weeks after LVAD implantation. Right upper quadrant ultrasound revealed no evidence of biliary obstruction. The LFTs normalized by the time of discharge from the hospital.
Discussion: The patient exhibited significant bilirubin elevation post-LVAD placement, with predominant direct bilirubinemia. Though the significant elevation of LDH and development of a hematoma requiring surgical evacuation suggest hemolysis as a potential contributor to hyperbilirubinemia, this does not explain the predominant direct hyperbilirubinemia. Intraoperative hypoxia or low cardiac output can cause liver injury, which may explain the increase in direct bilirubin. This case highlights the potential multifactorial etiology for hyperbilirubinemia following cardiac surgery.
Disclosures:
Pranav S. Ramamurthy, MD1, Victoria A. Caruso, DO2, Omar Haider, MD1, Jacob Alexander, MD, DM3. P3089 - An Intriguing Case of Direct Hyperbilirubinemia After Implantation of Left Ventricular Assist Device, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Massachusetts Chan Medical School - Baystate Medical Center, Springfield, MA; 2University of Massachusetts Chan Medical School - Baystate Medical Center, Windsor, CT; 3Baystate Medical Center, Springfield, MA
Introduction: Hyperbilirubinemia is well described after cardiac surgeries including implantation of left ventricular assist devices (LVAD) and has been found to be predictive of increased risk of morbidity and mortality. While intravascular hemolysis secondary to LVAD is often the primary mechanism for hyperbilirubinemia, we present a case that highlights the multifactorial origin of hyperbilirubinemia in this clinical situation.
Case Description/Methods: A 79-year-old male with a history of ischemic cardiomyopathy and aortic stenosis who was admitted with acute decompensated heart failure underwent implantation of LVAD and aortic valve replacement with bioprosthetic valve. The postoperative course was complicated by hypotension, coagulopathy and a mediastinal hematoma necessitating evacuation. He also required mechanical ventilation and multiple vasopressors which were eventually weaned off. His hemoglobin dropped to 7.8 g/dL post-operatively but recovered to 9.1 g/dL after transfusions. Electrolytes and creatinine remained normal. Lactate dehydrogenase peaked at 583 U/L. Liver function tests (LFTs) showed increasing total and direct bilirubin, peaking at 9.1 mg/dL and 7.3 mg/dL, respectively. Aspartate transaminase peaked at 215 U/L, alanine transaminase at 156 U/L and alkaline phosphatase at 204 U/L, three weeks after LVAD implantation. Right upper quadrant ultrasound revealed no evidence of biliary obstruction. The LFTs normalized by the time of discharge from the hospital.
Discussion: The patient exhibited significant bilirubin elevation post-LVAD placement, with predominant direct bilirubinemia. Though the significant elevation of LDH and development of a hematoma requiring surgical evacuation suggest hemolysis as a potential contributor to hyperbilirubinemia, this does not explain the predominant direct hyperbilirubinemia. Intraoperative hypoxia or low cardiac output can cause liver injury, which may explain the increase in direct bilirubin. This case highlights the potential multifactorial etiology for hyperbilirubinemia following cardiac surgery.
Disclosures:
Pranav Ramamurthy indicated no relevant financial relationships.
Victoria Caruso indicated no relevant financial relationships.
Omar Haider indicated no relevant financial relationships.
Jacob Alexander indicated no relevant financial relationships.
Pranav S. Ramamurthy, MD1, Victoria A. Caruso, DO2, Omar Haider, MD1, Jacob Alexander, MD, DM3. P3089 - An Intriguing Case of Direct Hyperbilirubinemia After Implantation of Left Ventricular Assist Device, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
