Monday Poster Session
Category: Liver
P3090 - Itchy Teen? Consider Genetic Intrahepatic Cholestatic Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jose A. Benitez, MD
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Jose A. Benitez, MD1, Francis Sharkey, MD1, Eugenia Tsai, MD1, Lisa Pedicone, PhD2, Jan Petrasek, MD, PhD1, Fabian Rodas, MD3, Andres Gomez-Aldana, MD2, Eric Lawitz, MD1, Fred Poordad, MD4, Carmen Landaverde, MD2
1University of Texas Health San Antonio, San Antonio, TX; 2Texas Liver Institute, San Antonio, TX; 3The Texas Liver Institute, San Antonio, TX; 4UTHSCSA, Texas Liver Institute, San Antonio, TX
Introduction: Progressive familial intrahepatic cholestasis (PFIC) refers to a group of rare genetic hepatobiliary diseases that impair bile secretion leading to cholestatic symptoms and clinical presentation. We present a case of PFIC type 3 diagnosed in a 15-year-old female.
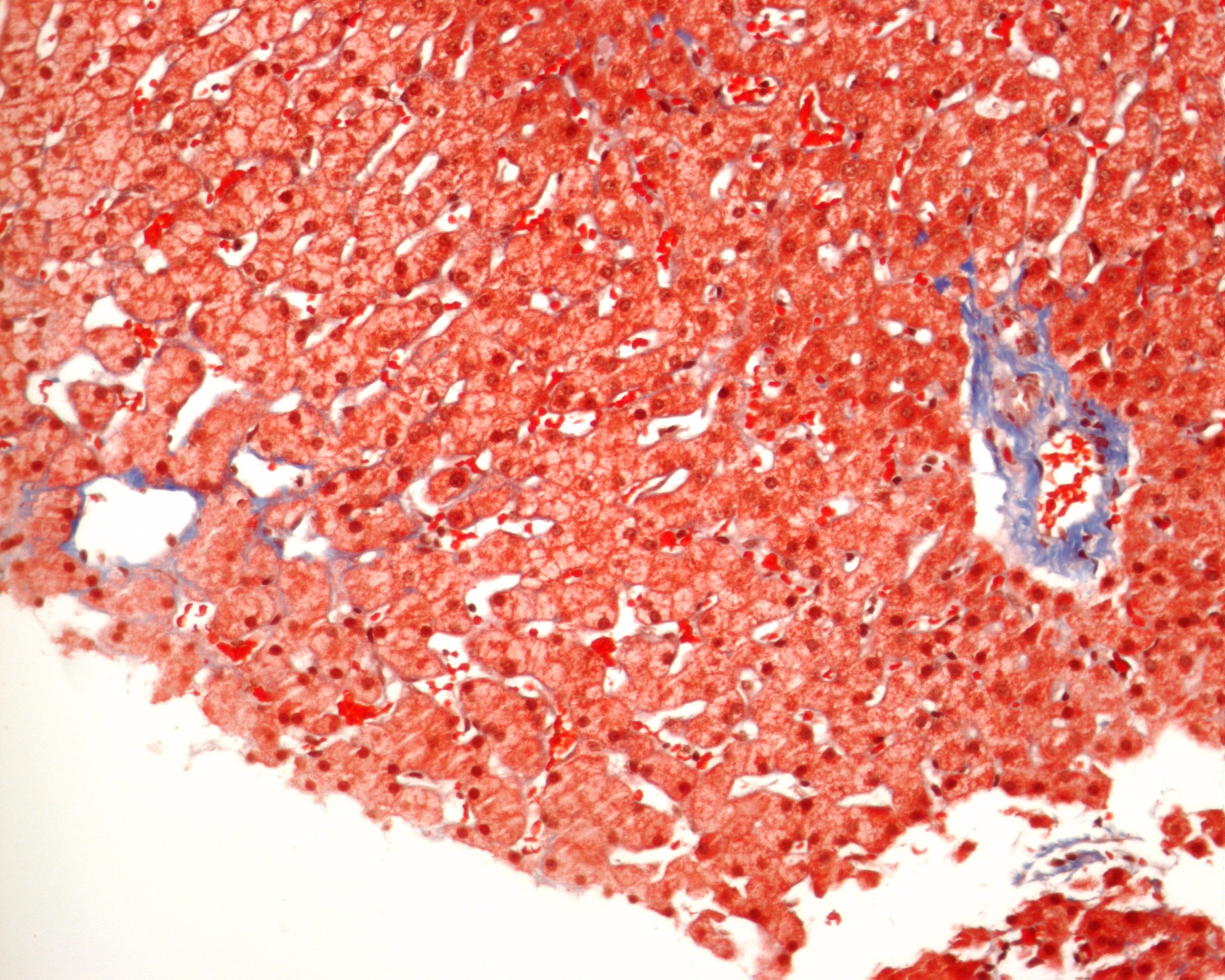
Case Description/Methods: A 15-year-old was brought in to her pediatrician for 5 weeks of pruritus and fatigue. She initially went to her PCP and an allergist with no resolution of symptoms. Her CBC and mono test were negative, however, LFTs were elevated, AST of 80 and ALT 170. Bilirubin, alkaline phosphatase, and albumin were normal at the time. Labs prompted peds GI consult to workup possible liver disease. Liver biopsy showed ductopenia but no fibrosis nor lesions (Figure 1). Additionally, workup through a jaundice chip showed a heterozygous mutation in the ABCB4, so patient was subsequently diagnosed with PFIC type 3. Despite several dosage increments in ursodiol, patient continued with severe pruritus but stable LFTs, therefore odevixibat was prescribed. This new medication, used concomitantly with ursodiol, helped alleviate her symptoms, however due to GI side effects, dose was halved from 2400 to 1200 mg daily. Patient was also started on cholestyramine PRN with subjective improvement reported afterwards, however AST/ALT remained elevated similar to baseline.
Discussion: PFIC is a rare genetic disorder that impairs biliary secretion leading to cholestatic symptoms. Specific genetic variants in the well-known PFIC genes (ABCB4, ABCB11, and ATP8B1) can contribute to the development of cholestatic phenotypes later in life, even in adults.
PFIC diagnosis relies on a combination of clinical evaluation, chronic pruritus being a pivotal symptom, alongside genetic testing and liver biopsy. Once confirmed, pharmacotherapy is the initial treatment approach, primarily targeting the prevention of long-term complications and improving quality of life. Ursodiol (ursodeoxycholic acid) is the first-line medication, though its effectiveness can be variable. Other options include rifampicin for pruritus relief and cholestyramine to bind bile acids. Newer drugs known as ileal bile acid transporter inhibitors (IBATi), such as odevixibat, can significantly decrease serum bile acid levels and improve pruritus in patients with PFIC. Due to increased risk of cirrhosis, early diagnosis is crucial for patients with PFIC. This emphasizes the importance of heightened awareness of this disease, which can present in the teenage years or later in life.
Disclosures:
Jose A. Benitez, MD1, Francis Sharkey, MD1, Eugenia Tsai, MD1, Lisa Pedicone, PhD2, Jan Petrasek, MD, PhD1, Fabian Rodas, MD3, Andres Gomez-Aldana, MD2, Eric Lawitz, MD1, Fred Poordad, MD4, Carmen Landaverde, MD2. P3090 - Itchy Teen? Consider Genetic Intrahepatic Cholestatic Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health San Antonio, San Antonio, TX; 2Texas Liver Institute, San Antonio, TX; 3The Texas Liver Institute, San Antonio, TX; 4UTHSCSA, Texas Liver Institute, San Antonio, TX
Introduction: Progressive familial intrahepatic cholestasis (PFIC) refers to a group of rare genetic hepatobiliary diseases that impair bile secretion leading to cholestatic symptoms and clinical presentation. We present a case of PFIC type 3 diagnosed in a 15-year-old female.
Case Description/Methods: A 15-year-old was brought in to her pediatrician for 5 weeks of pruritus and fatigue. She initially went to her PCP and an allergist with no resolution of symptoms. Her CBC and mono test were negative, however, LFTs were elevated, AST of 80 and ALT 170. Bilirubin, alkaline phosphatase, and albumin were normal at the time. Labs prompted peds GI consult to workup possible liver disease. Liver biopsy showed ductopenia but no fibrosis nor lesions (Figure 1). Additionally, workup through a jaundice chip showed a heterozygous mutation in the ABCB4, so patient was subsequently diagnosed with PFIC type 3. Despite several dosage increments in ursodiol, patient continued with severe pruritus but stable LFTs, therefore odevixibat was prescribed. This new medication, used concomitantly with ursodiol, helped alleviate her symptoms, however due to GI side effects, dose was halved from 2400 to 1200 mg daily. Patient was also started on cholestyramine PRN with subjective improvement reported afterwards, however AST/ALT remained elevated similar to baseline.
Discussion: PFIC is a rare genetic disorder that impairs biliary secretion leading to cholestatic symptoms. Specific genetic variants in the well-known PFIC genes (ABCB4, ABCB11, and ATP8B1) can contribute to the development of cholestatic phenotypes later in life, even in adults.
PFIC diagnosis relies on a combination of clinical evaluation, chronic pruritus being a pivotal symptom, alongside genetic testing and liver biopsy. Once confirmed, pharmacotherapy is the initial treatment approach, primarily targeting the prevention of long-term complications and improving quality of life. Ursodiol (ursodeoxycholic acid) is the first-line medication, though its effectiveness can be variable. Other options include rifampicin for pruritus relief and cholestyramine to bind bile acids. Newer drugs known as ileal bile acid transporter inhibitors (IBATi), such as odevixibat, can significantly decrease serum bile acid levels and improve pruritus in patients with PFIC. Due to increased risk of cirrhosis, early diagnosis is crucial for patients with PFIC. This emphasizes the importance of heightened awareness of this disease, which can present in the teenage years or later in life.
Figure: Figure 1: Liver biopsy showing central vein (arrow A – note open sinusoids and lack of cholestasis) and a portal tract (arrow B – note lack of bile duct). (Trichrome, x200)
Dr. Frank Sharkey
Dr. Frank Sharkey
Disclosures:
Jose Benitez indicated no relevant financial relationships.
Francis Sharkey indicated no relevant financial relationships.
Eugenia Tsai indicated no relevant financial relationships.
Lisa Pedicone indicated no relevant financial relationships.
Jan Petrasek indicated no relevant financial relationships.
Fabian Rodas indicated no relevant financial relationships.
Andres Gomez-Aldana indicated no relevant financial relationships.
Eric Lawitz indicated no relevant financial relationships.
Fred Poordad indicated no relevant financial relationships.
Carmen Landaverde indicated no relevant financial relationships.
Jose A. Benitez, MD1, Francis Sharkey, MD1, Eugenia Tsai, MD1, Lisa Pedicone, PhD2, Jan Petrasek, MD, PhD1, Fabian Rodas, MD3, Andres Gomez-Aldana, MD2, Eric Lawitz, MD1, Fred Poordad, MD4, Carmen Landaverde, MD2. P3090 - Itchy Teen? Consider Genetic Intrahepatic Cholestatic Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
