Monday Poster Session
Category: Liver
P3097 - The Case of Life-Threatening Hepatitis: Ceftriaxone-Induced Severe Liver Injury
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Shalva Eliava, MD
Englewood Hospital and Medical Center
Englewood, NJ
Presenting Author(s)
Shalva Eliava, MD1, Chadane Thompson, MD1, Danielle Pope, MD2, Ross T. Lavine, MD1
1Englewood Hospital and Medical Center, Englewood, NJ; 2Englewood Hospital and Medical Center, Bogota, NJ
Introduction: Ceftriaxone is one of the most commonly used antibiotics in clinical practice. Cholestasis and hepatitis are well-known adverse reactions, typically manifesting as mild or self-limited derangements in the days to weeks following drug initiation. We present a rare case of severe hepatitis associated with ceftriaxone use.
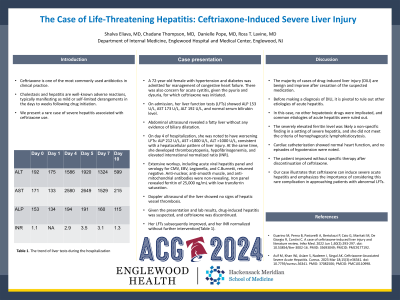
Case Description/Methods: A 72-year-old female with hypertension and diabetes was admitted for management of congestive heart failure. There was also concern for acute cystitis, given the pyuria and dysuria, for which ceftriaxone was initiated. On admission, her liver function tests (LFTs) showed ALP 153 U/L, AST 173 U/L, ALT 192 U/L, and serum bilirubin level. Abdominal ultrasound revealed a fatty liver without any evidence of biliary dilatation. On day 4 of hospitalization, she was noted to have worsening LFTs: ALP 212 U/L, AST >1000 U/L, ALT >1000 U/L, consistent with a hepatocellular pattern of liver injury. At the same time, she developed thrombocytopenia, hypofibrinogenemia, and elevated international normalized ratio (INR). Extensive workup, including acute viral hepatitis panel and serology for CMV, EBV, Legionella, and C.Burnetii, returned negative. Anti-nuclear, anti-smooth muscle, and anti-mitochondrial antibodies were non-revealing. Iron panel revealed ferritin of 25,000 ng/mL with low transferrin saturation. Doppler ultrasound of the liver showed no signs of hepatic vessel thrombosis. Given the presentation and lab results, drug-induced hepatitis was suspected, and ceftriaxone was discontinued. Her LFTs subsequently improved, and her INR normalized without further intervention(Table 1).
Discussion: The majority of cases of drug-induced liver injury (DILI) are benign and improve after cessation of the suspected medication. Before making a diagnosis of DILI, it is pivotal to rule out other etiologies of acute hepatitis. In this case, no other hepatotoxic drugs were implicated, and common etiologies of acute hepatitis were ruled out. The severely elevated ferritin level was likely a non-specific finding in a setting of severe hepatitis, and she did not meet the criteria of hemophagocytic lymphohistiocytosis. Cardiac catheterization showed normal heart function, and no episodes of hypotension were noted. The patient improved without specific therapy after discontinuation of ceftriaxone. Our case illustrates that ceftriaxone can induce severe acute hepatitis and emphasizes the importance of considering this rare complication in approaching patients with abnormal LFTs.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Shalva Eliava, MD1, Chadane Thompson, MD1, Danielle Pope, MD2, Ross T. Lavine, MD1. P3097 - The Case of Life-Threatening Hepatitis: Ceftriaxone-Induced Severe Liver Injury, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Englewood Hospital and Medical Center, Englewood, NJ; 2Englewood Hospital and Medical Center, Bogota, NJ
Introduction: Ceftriaxone is one of the most commonly used antibiotics in clinical practice. Cholestasis and hepatitis are well-known adverse reactions, typically manifesting as mild or self-limited derangements in the days to weeks following drug initiation. We present a rare case of severe hepatitis associated with ceftriaxone use.
Case Description/Methods: A 72-year-old female with hypertension and diabetes was admitted for management of congestive heart failure. There was also concern for acute cystitis, given the pyuria and dysuria, for which ceftriaxone was initiated. On admission, her liver function tests (LFTs) showed ALP 153 U/L, AST 173 U/L, ALT 192 U/L, and serum bilirubin level. Abdominal ultrasound revealed a fatty liver without any evidence of biliary dilatation. On day 4 of hospitalization, she was noted to have worsening LFTs: ALP 212 U/L, AST >1000 U/L, ALT >1000 U/L, consistent with a hepatocellular pattern of liver injury. At the same time, she developed thrombocytopenia, hypofibrinogenemia, and elevated international normalized ratio (INR). Extensive workup, including acute viral hepatitis panel and serology for CMV, EBV, Legionella, and C.Burnetii, returned negative. Anti-nuclear, anti-smooth muscle, and anti-mitochondrial antibodies were non-revealing. Iron panel revealed ferritin of 25,000 ng/mL with low transferrin saturation. Doppler ultrasound of the liver showed no signs of hepatic vessel thrombosis. Given the presentation and lab results, drug-induced hepatitis was suspected, and ceftriaxone was discontinued. Her LFTs subsequently improved, and her INR normalized without further intervention(Table 1).
Discussion: The majority of cases of drug-induced liver injury (DILI) are benign and improve after cessation of the suspected medication. Before making a diagnosis of DILI, it is pivotal to rule out other etiologies of acute hepatitis. In this case, no other hepatotoxic drugs were implicated, and common etiologies of acute hepatitis were ruled out. The severely elevated ferritin level was likely a non-specific finding in a setting of severe hepatitis, and she did not meet the criteria of hemophagocytic lymphohistiocytosis. Cardiac catheterization showed normal heart function, and no episodes of hypotension were noted. The patient improved without specific therapy after discontinuation of ceftriaxone. Our case illustrates that ceftriaxone can induce severe acute hepatitis and emphasizes the importance of considering this rare complication in approaching patients with abnormal LFTs.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Shalva Eliava indicated no relevant financial relationships.
Chadane Thompson indicated no relevant financial relationships.
Danielle Pope indicated no relevant financial relationships.
Ross Lavine indicated no relevant financial relationships.
Shalva Eliava, MD1, Chadane Thompson, MD1, Danielle Pope, MD2, Ross T. Lavine, MD1. P3097 - The Case of Life-Threatening Hepatitis: Ceftriaxone-Induced Severe Liver Injury, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
