Monday Poster Session
Category: Liver
P3101 - Left Ventricular Assist Device as a Possible Instrument for Reversing Liver Fibrosis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Nina Quirk, MS, MD
University of Texas Health, McGovern Medical School
Houston, TX
Presenting Author(s)
Award: Presidential Poster Award
Nina Quirk, MS, MD, Yllen Hernandez Blanco, MD, Akshata Moghe, MD, PhD, Erin Rubin, MD, Victor Machicao, MD
University of Texas Health, McGovern Medical School, Houston, TX
Introduction: Heart failure (HF) is a common global condition with high mortality rates. End organ dysfunction is the major complication of acute decompensated heart failure (AdHF) and end-stage HF. The liver is an affected organ with presumed multifactorial etiology of inflammatory hepatopathy, ischemic hepatitis, and congestive hepatopathy. One intervention that has been shown to improve organ function is left ventricular assist device (LVAD). There are few studies regarding resolution or improvement of hepatic fibrosis post- LVAD placement.
Case Description/Methods: We present a case of a 68-year-old female with history of chronic obstructive pulmonary disease, hypertension, atrial fibrillation, cocaine abuse, hepatitis C treated with Peginterferon alpha, myocardial infarction status post percutaneous coronary intervention to proximal and middle left anterior descending artery, HF with reduced ejection fraction (25-30%) with mixed cardiomyopathy. Hepatology was consulted for ‘clearance’ for LVAD placement. At that time, liver enzymes showed an aspartate aminotransferase (AST) of 40 and alanine aminotransferase (ALT) of 44 with preserved synthetic function. Ultrasound elastography with Fibrosure showed F2-F3 fibrosis (9.6 kPa) and liver biopsy showed centrilobular mild sinusoidal dilation and hepatocyte cord atrophy with perivenular, perisinusoidal and periportal fibrosis, stage 2, with moderate iron accumulation.
The patient subsequently underwent LVAD placement with normalization of liver enzymes and synthetic function. Fibrosure suggested F1 fibrosis. Repeat trans-jugular liver biopsy showed minimal lipofuscin pigment deposition with no fibrosis, no steatosis, and no congestion. The patient is currently pending cardiac transplant.
Discussion: LVAD placement has shown promising resolution of hepatic and renal function. Improvement in portal vein flow volume and velocity as well as serum markers of hepatic and biliary function has also been observed. In this case, resolution of hepatic fibrosis was seen.
Liver dysfunction is associated with worse survival post-heart transplant. Patients with advanced heart failure and liver dysfunction (reflected by high MELD score) have worse survival post-heart transplant.Thus, there is merit in trying to improve or reverse liver dysfunction to improve survival outcomes in this patient population.
Further studies are needed to risk stratify patients with different, especially higher stages of fibrosis, as well as compensated cirrhosis, for outcomes post-LVAD placement.
Disclosures:
Nina Quirk, MS, MD, Yllen Hernandez Blanco, MD, Akshata Moghe, MD, PhD, Erin Rubin, MD, Victor Machicao, MD. P3101 - Left Ventricular Assist Device as a Possible Instrument for Reversing Liver Fibrosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Nina Quirk, MS, MD, Yllen Hernandez Blanco, MD, Akshata Moghe, MD, PhD, Erin Rubin, MD, Victor Machicao, MD
University of Texas Health, McGovern Medical School, Houston, TX
Introduction: Heart failure (HF) is a common global condition with high mortality rates. End organ dysfunction is the major complication of acute decompensated heart failure (AdHF) and end-stage HF. The liver is an affected organ with presumed multifactorial etiology of inflammatory hepatopathy, ischemic hepatitis, and congestive hepatopathy. One intervention that has been shown to improve organ function is left ventricular assist device (LVAD). There are few studies regarding resolution or improvement of hepatic fibrosis post- LVAD placement.
Case Description/Methods: We present a case of a 68-year-old female with history of chronic obstructive pulmonary disease, hypertension, atrial fibrillation, cocaine abuse, hepatitis C treated with Peginterferon alpha, myocardial infarction status post percutaneous coronary intervention to proximal and middle left anterior descending artery, HF with reduced ejection fraction (25-30%) with mixed cardiomyopathy. Hepatology was consulted for ‘clearance’ for LVAD placement. At that time, liver enzymes showed an aspartate aminotransferase (AST) of 40 and alanine aminotransferase (ALT) of 44 with preserved synthetic function. Ultrasound elastography with Fibrosure showed F2-F3 fibrosis (9.6 kPa) and liver biopsy showed centrilobular mild sinusoidal dilation and hepatocyte cord atrophy with perivenular, perisinusoidal and periportal fibrosis, stage 2, with moderate iron accumulation.
The patient subsequently underwent LVAD placement with normalization of liver enzymes and synthetic function. Fibrosure suggested F1 fibrosis. Repeat trans-jugular liver biopsy showed minimal lipofuscin pigment deposition with no fibrosis, no steatosis, and no congestion. The patient is currently pending cardiac transplant.
Discussion: LVAD placement has shown promising resolution of hepatic and renal function. Improvement in portal vein flow volume and velocity as well as serum markers of hepatic and biliary function has also been observed. In this case, resolution of hepatic fibrosis was seen.
Liver dysfunction is associated with worse survival post-heart transplant. Patients with advanced heart failure and liver dysfunction (reflected by high MELD score) have worse survival post-heart transplant.Thus, there is merit in trying to improve or reverse liver dysfunction to improve survival outcomes in this patient population.
Further studies are needed to risk stratify patients with different, especially higher stages of fibrosis, as well as compensated cirrhosis, for outcomes post-LVAD placement.
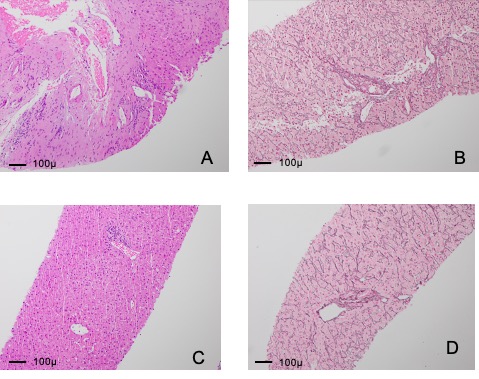
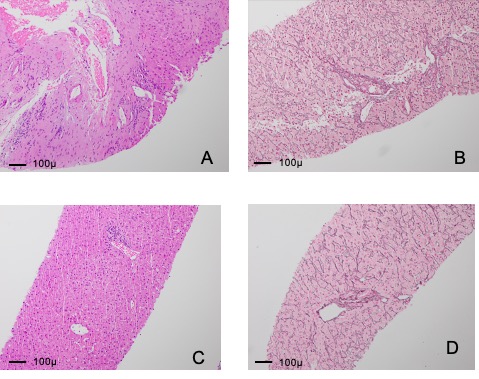
Figure: Image A: Large portal tract H&E stain 10x, pre-LVAD. Image B: Small portal tract reticulin stain x10, pre-LVAD. The microscopic examination of the fragmented cores of hepatic tissue pre-LVAD placement shows architectural remodeling with findings of vascular flow abnormality. Images A and B show early nodular regenerative hyperplasia with branching of the portal venules. Alternations of hepatic blood flow, such as in advanced heart failure, result in architectural remodeling with atrophy and hypertrophy of the hepatic parenchyma.
Image C: Portal tract H&E stain 10x, post-LVAD. Image D: Small portal tract reticulin stain 10x, post-LVAD. Image C shows the resolution of architecture abnormalities and demonstrates normal relationship of portal tract to central vein. There is also no longer compression of hepatic cell plates as seen in Image D.
Image C: Portal tract H&E stain 10x, post-LVAD. Image D: Small portal tract reticulin stain 10x, post-LVAD. Image C shows the resolution of architecture abnormalities and demonstrates normal relationship of portal tract to central vein. There is also no longer compression of hepatic cell plates as seen in Image D.
Disclosures:
Nina Quirk indicated no relevant financial relationships.
Yllen Hernandez Blanco indicated no relevant financial relationships.
Akshata Moghe: Alnylam – Consultant. Recordati Rare Dis Inc. – Consultant.
Erin Rubin indicated no relevant financial relationships.
Victor Machicao indicated no relevant financial relationships.
Nina Quirk, MS, MD, Yllen Hernandez Blanco, MD, Akshata Moghe, MD, PhD, Erin Rubin, MD, Victor Machicao, MD. P3101 - Left Ventricular Assist Device as a Possible Instrument for Reversing Liver Fibrosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

