Monday Poster Session
Category: Liver
P3103 - Postoperative Sequelae in Giant Cavernous Hemangioma: Recurrent Cholangitis and Enlargement of Residual Hemangioma Following Hepatic Lobectomy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- TN
Toru Nakata, MD, PhD
University of Hawaii, John A. Burns School of Medicine
Honolulu, HI
Presenting Author(s)
Toru Nakata, MD, PhD1, Arvin Jeremy Tan, MD1, Tomoki Sempokuya, MD2, Chuong Tran, MD3
1University of Hawaii, John A. Burns School of Medicine, Honolulu, HI; 2University of Hawaii, Honolulu, HI; 3John A. Burns School of Medicine, University of Hawaii, Honolulu, HI
Introduction: Hepatic cavernous hemangiomas are the most common benign hepatic tumors, with a prevalence of 4-20% (1). Surgical intervention is warranted for managing giant hemangiomas, especially when faced with risks such as rupture, bleeding, thrombosis, or Kasabach-Merritt Syndrome (2). Nonetheless, reports on complications post-hepatic lobectomy remain scarce. We present a case of a patient with a giant cavernous hemangioma who underwent a right partial hepatic lobectomy and subsequently developed a biliary stricture, coupled with the enlargement of a residual hemangioma in the left hepatic lobe.
Case Description/Methods: A 39-year-old male with past medical history for giant cavernous hemangioma status post right partial hepatic lobectomy, who was referred to our hospital for intermittent fever and abnormal liver function tests (LFTs).
Six years ago, the patient was diagnosed with a giant hepatic cavernous hemangioma weighing 17 lbs and underwent a right partial lobectomy with hepaticojejunostomy. Post-surgery, he experienced recurrent sepsis and cholangitis, requiring 13 procedures to address biliary duct strictures. Five years ago, an attempt to remove an internal biliary stent failed. The patient relocated to current residence four years ago for further management and remained symptom-free until this February, when abnormal LFTs (AST 163, ALT 232, ALP 440, T-bil 0.7) prompted a referral to our hospital.
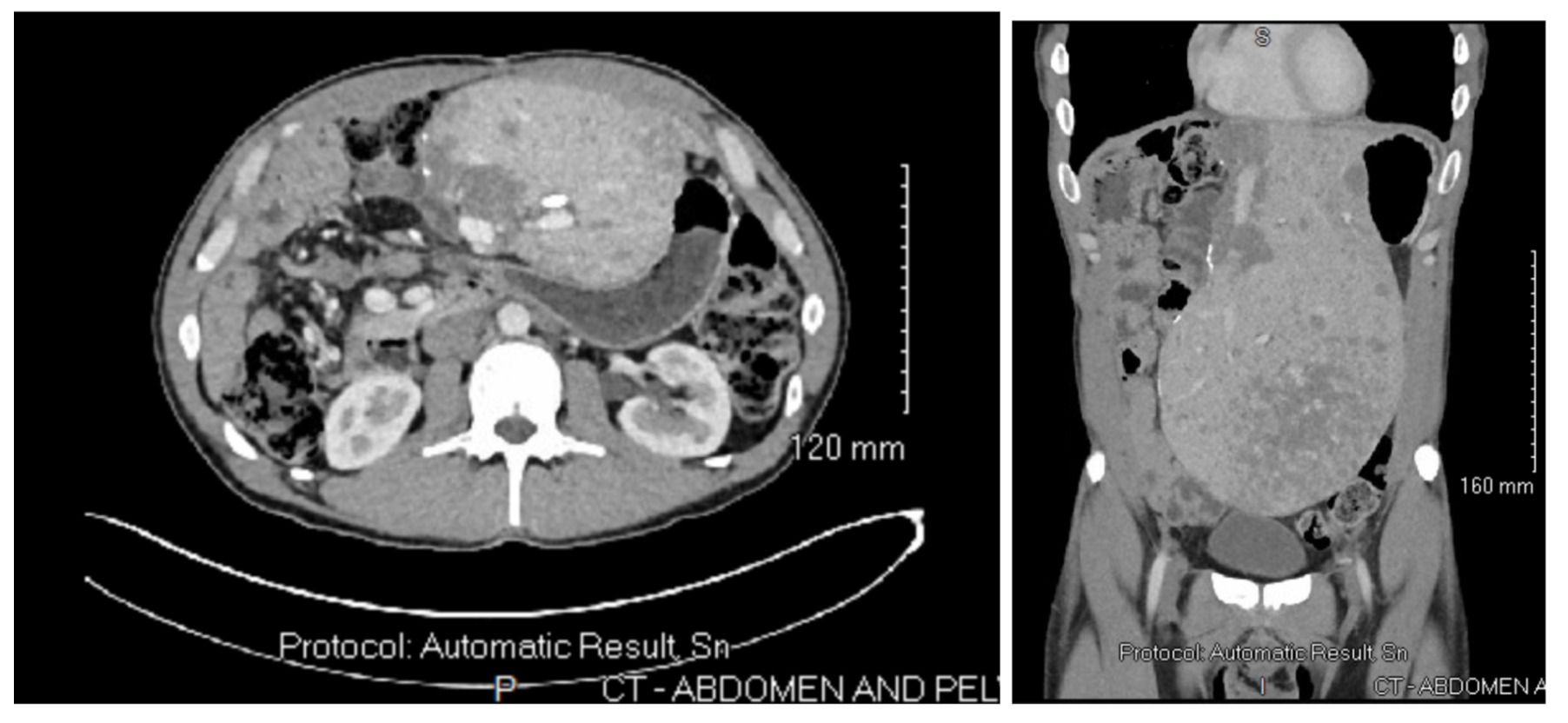
On admission, he presented with intermittent fever and worsening of LFTs (AST 402, ALT 527, ALP 978, T-bil 0.6), without leukocytosis, or thrombocytosis. Viral hepatitis panel was negative. A CT scan revealed partial right hepatectomy with compensatory hypertrophy of the left hepatic lobe (27 x 17 cm) and numerous hepatic hypodensities (Fig.1). MRCP showed post-surgical changes without biliary dilation and numerous liver lesions likely representing hemangiomas.
After initiating antibiotics and placing internal and external biliary drains in the left biliary tract via interventional radiology, the patient's LFTs had improved. The retained stent was successfully removed via balloon cholangioplasty. Following significant improvement, the patient was discharged after six days.
Discussion: The current admission reveals a biliary stricture and an enlarged residual hemangioma in the left hepatic lobe, raising concerns of potential complications such as bleeding, rupture, or Kasabach-Merritt Syndrome, necessitating vigilant monitoring and possible consideration of liver transplantation in critical cases.
Disclosures:
Toru Nakata, MD, PhD1, Arvin Jeremy Tan, MD1, Tomoki Sempokuya, MD2, Chuong Tran, MD3. P3103 - Postoperative Sequelae in Giant Cavernous Hemangioma: Recurrent Cholangitis and Enlargement of Residual Hemangioma Following Hepatic Lobectomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Hawaii, John A. Burns School of Medicine, Honolulu, HI; 2University of Hawaii, Honolulu, HI; 3John A. Burns School of Medicine, University of Hawaii, Honolulu, HI
Introduction: Hepatic cavernous hemangiomas are the most common benign hepatic tumors, with a prevalence of 4-20% (1). Surgical intervention is warranted for managing giant hemangiomas, especially when faced with risks such as rupture, bleeding, thrombosis, or Kasabach-Merritt Syndrome (2). Nonetheless, reports on complications post-hepatic lobectomy remain scarce. We present a case of a patient with a giant cavernous hemangioma who underwent a right partial hepatic lobectomy and subsequently developed a biliary stricture, coupled with the enlargement of a residual hemangioma in the left hepatic lobe.
Case Description/Methods: A 39-year-old male with past medical history for giant cavernous hemangioma status post right partial hepatic lobectomy, who was referred to our hospital for intermittent fever and abnormal liver function tests (LFTs).
Six years ago, the patient was diagnosed with a giant hepatic cavernous hemangioma weighing 17 lbs and underwent a right partial lobectomy with hepaticojejunostomy. Post-surgery, he experienced recurrent sepsis and cholangitis, requiring 13 procedures to address biliary duct strictures. Five years ago, an attempt to remove an internal biliary stent failed. The patient relocated to current residence four years ago for further management and remained symptom-free until this February, when abnormal LFTs (AST 163, ALT 232, ALP 440, T-bil 0.7) prompted a referral to our hospital.
On admission, he presented with intermittent fever and worsening of LFTs (AST 402, ALT 527, ALP 978, T-bil 0.6), without leukocytosis, or thrombocytosis. Viral hepatitis panel was negative. A CT scan revealed partial right hepatectomy with compensatory hypertrophy of the left hepatic lobe (27 x 17 cm) and numerous hepatic hypodensities (Fig.1). MRCP showed post-surgical changes without biliary dilation and numerous liver lesions likely representing hemangiomas.
After initiating antibiotics and placing internal and external biliary drains in the left biliary tract via interventional radiology, the patient's LFTs had improved. The retained stent was successfully removed via balloon cholangioplasty. Following significant improvement, the patient was discharged after six days.
Discussion: The current admission reveals a biliary stricture and an enlarged residual hemangioma in the left hepatic lobe, raising concerns of potential complications such as bleeding, rupture, or Kasabach-Merritt Syndrome, necessitating vigilant monitoring and possible consideration of liver transplantation in critical cases.
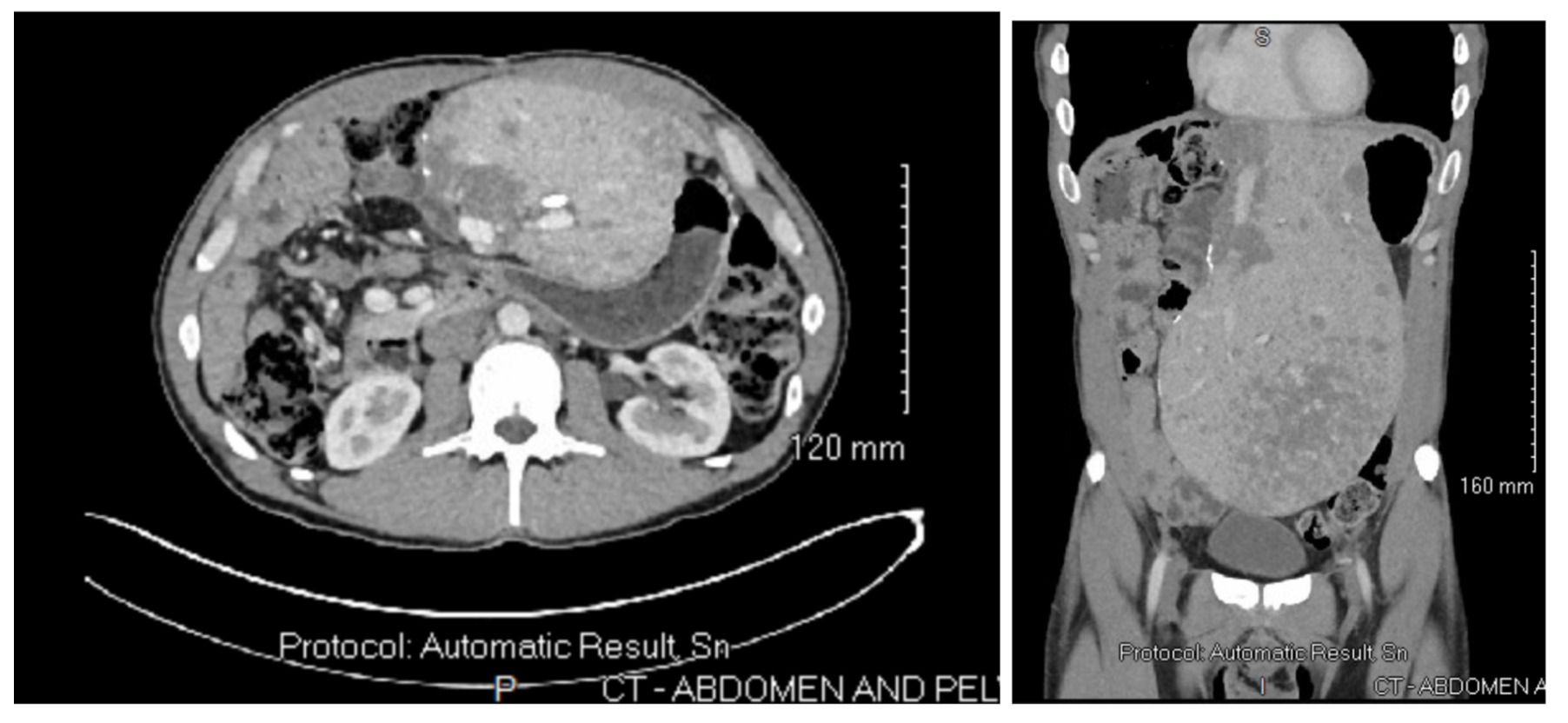
Figure: Fig.1 Hepatic cavenous hemangioma and massively enlarged left hepatic lobe. (Left) Transverse view and (Right) Coronal View.
Disclosures:
Toru Nakata indicated no relevant financial relationships.
Arvin Jeremy Tan indicated no relevant financial relationships.
Tomoki Sempokuya indicated no relevant financial relationships.
Chuong Tran indicated no relevant financial relationships.
Toru Nakata, MD, PhD1, Arvin Jeremy Tan, MD1, Tomoki Sempokuya, MD2, Chuong Tran, MD3. P3103 - Postoperative Sequelae in Giant Cavernous Hemangioma: Recurrent Cholangitis and Enlargement of Residual Hemangioma Following Hepatic Lobectomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
