Monday Poster Session
Category: Liver
P3018 - A Rare Case of Propofol-Induced Liver Injury
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Dhruv Patel, MD, MBA
HCA Healthcare
Houston, TX
Presenting Author(s)
Suhas Kandimalla, MD1, Dhruv Patel, MD, MBA2, Jeby Kalathoor, MD2, Diane Habib, MD1, George Elias, MD2
1HCA Healthcare, Spring, TX; 2HCA Healthcare, Kingwood, TX
Introduction: Drug-induced liver injury (DILI), often causing acute liver failure, is typically immune-mediated and linked to human leukocyte antigen variants. Diagnosis requires high clinical suspicion and exclusion of other common causes of liver damage. We report a rare case of propofol-induced liver injury.
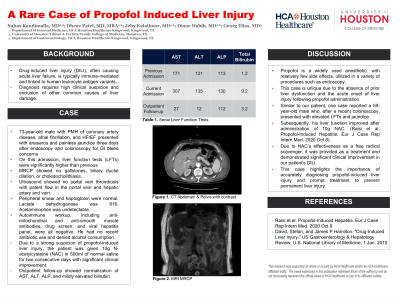
Case Description/Methods: A 73-year-old male with a history of coronary artery disease, atrial fibrillation, and heart failure with reduced ejection fraction presented with anasarca and painless jaundice. The week prior, he had undergone an endoscopy and colonoscopy for concerns of a gastrointestinal bleed. On admission, liver function tests (LFTs) showed total bilirubin of 9.2, aspartate aminotransferase (AST) of 307, alanine transaminase (ALT) of 135, and alkaline phosphatase (ALP) of 130. Magnetic resonance cholangiopancreatography revealed no gallstones, biliary ductal dilation, or choledocholithiasis. Ultrasound showed no portal vein thrombosis with patent flow in the portal vein and hepatic artery and vein. Peripheral smear and haptoglobin were normal. Lactate dehydrogenase was 816. Acetaminophen was undetectable. Autoimmune workup, including anti-mitochondrial and anti-smooth muscle antibodies, drug screen, and viral hepatitis panel, were all negative. He had no recent antibiotic use and denied alcohol consumption. Due to a strong suspicion of propofol-induced liver injury, the patient was given 10g N-acetylcysteine (NAC) in 500ml of normal saline for two days with significant clinical improvement. Outpatient follow-up showed normalization of AST, ALT, ALP, and mildly elevated bilirubin.
Discussion: Propofol is a widely used anesthetic, with relatively few side effects, utilized in a variety of procedures such as endoscopy. This case is unique due to the absence of prior liver dysfunction and the acute onset of liver injury following propofol administration. Similar to our patient, one case reported a 59-year-old male who, after a recent colonoscopy, presented with elevated LFTs and jaundice. Subsequently, his liver function improved after administration of 10g NAC. (Raisi et al, Propofol-Induced Hepatitis. Eur J Case Rep Intern Med. 2020 Oct 8). Due to NAC’s effectiveness as a free radical scavenger, it was provided as a treatment and demonstrated significant clinical improvement in our patient's DILI. This case highlights the importance of accurately diagnosing propofol-induced liver injury and prompt treatment to prevent permanent liver injury.
Disclosures:
Suhas Kandimalla, MD1, Dhruv Patel, MD, MBA2, Jeby Kalathoor, MD2, Diane Habib, MD1, George Elias, MD2. P3018 - A Rare Case of Propofol-Induced Liver Injury, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1HCA Healthcare, Spring, TX; 2HCA Healthcare, Kingwood, TX
Introduction: Drug-induced liver injury (DILI), often causing acute liver failure, is typically immune-mediated and linked to human leukocyte antigen variants. Diagnosis requires high clinical suspicion and exclusion of other common causes of liver damage. We report a rare case of propofol-induced liver injury.
Case Description/Methods: A 73-year-old male with a history of coronary artery disease, atrial fibrillation, and heart failure with reduced ejection fraction presented with anasarca and painless jaundice. The week prior, he had undergone an endoscopy and colonoscopy for concerns of a gastrointestinal bleed. On admission, liver function tests (LFTs) showed total bilirubin of 9.2, aspartate aminotransferase (AST) of 307, alanine transaminase (ALT) of 135, and alkaline phosphatase (ALP) of 130. Magnetic resonance cholangiopancreatography revealed no gallstones, biliary ductal dilation, or choledocholithiasis. Ultrasound showed no portal vein thrombosis with patent flow in the portal vein and hepatic artery and vein. Peripheral smear and haptoglobin were normal. Lactate dehydrogenase was 816. Acetaminophen was undetectable. Autoimmune workup, including anti-mitochondrial and anti-smooth muscle antibodies, drug screen, and viral hepatitis panel, were all negative. He had no recent antibiotic use and denied alcohol consumption. Due to a strong suspicion of propofol-induced liver injury, the patient was given 10g N-acetylcysteine (NAC) in 500ml of normal saline for two days with significant clinical improvement. Outpatient follow-up showed normalization of AST, ALT, ALP, and mildly elevated bilirubin.
Discussion: Propofol is a widely used anesthetic, with relatively few side effects, utilized in a variety of procedures such as endoscopy. This case is unique due to the absence of prior liver dysfunction and the acute onset of liver injury following propofol administration. Similar to our patient, one case reported a 59-year-old male who, after a recent colonoscopy, presented with elevated LFTs and jaundice. Subsequently, his liver function improved after administration of 10g NAC. (Raisi et al, Propofol-Induced Hepatitis. Eur J Case Rep Intern Med. 2020 Oct 8). Due to NAC’s effectiveness as a free radical scavenger, it was provided as a treatment and demonstrated significant clinical improvement in our patient's DILI. This case highlights the importance of accurately diagnosing propofol-induced liver injury and prompt treatment to prevent permanent liver injury.
Disclosures:
Suhas Kandimalla indicated no relevant financial relationships.
Dhruv Patel indicated no relevant financial relationships.
Jeby Kalathoor indicated no relevant financial relationships.
Diane Habib indicated no relevant financial relationships.
George Elias indicated no relevant financial relationships.
Suhas Kandimalla, MD1, Dhruv Patel, MD, MBA2, Jeby Kalathoor, MD2, Diane Habib, MD1, George Elias, MD2. P3018 - A Rare Case of Propofol-Induced Liver Injury, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
