Monday Poster Session
Category: Liver
P3019 - Biliary Obstruction from Transjugular Intrahepatic Portosystemic Shunt Mimicking Alcohol-Associated Hepatitis - A Rare Complication
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Yash Hegde, MD
University of Wisconsin School of Medicine and Public Health
Madison, WI
Presenting Author(s)
Yash Hegde, MD1, Dana A. Ley, MD2, Adnan Said, MD, MS2, Prasad Dalvie, MD1, Mark Benson, MD1, Deepak V. Gopal, MD, FACG2
1University of Wisconsin School of Medicine and Public Health, Madison, WI; 2University of Wisconsin Hospitals and Clinics, Madison, WI
Introduction: Transjugular intrahepatic portosystemic shunt (TIPS) is a procedure used to decrease portal hypertension. The two most common clinical indications for TIPS include secondary prevention of variceal hemorrhage and refractory ascites. Biliary complications, most commonly biliary-shunt fistula formation, remain relatively rare. Biliary obstruction secondary to TIPS placement is a rare complication, with few cases reported in the literature.
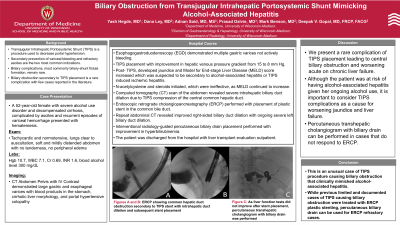
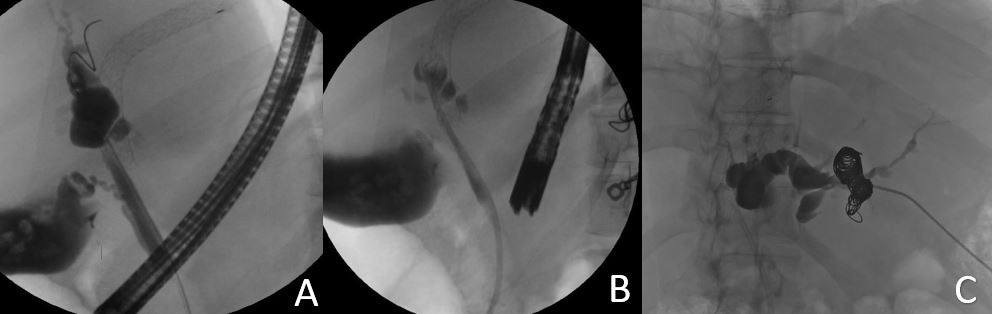
Case Description/Methods: A 52-year-old female with alcohol use disorder and decompensated alcohol-related cirrhosis, complicated by portal hypertension with ascites and recurrent episodes of variceal hemorrhage despite variceal band ligation, presented with hematemesis. Her blood alcohol level was significantly elevated at 300 mg/dL. Esophagogastroduodenoscopy (EGD) demonstrated multiple gastric varices secondary to portal hypertension, not actively bleeding. She underwent TIPS placement with improvement in hepatic venous pressure gradient from 15 to 8 mm Hg. Post-TIPS, her Model for End-stage Liver Disease (MELD) score increased which was suspected to be secondary to alcohol-associated hepatitis or TIPS induced ischemic hepatitis. She was started on N-acetylcysteine and steroids, which were ineffective, as demonstrated by continued increase in MELD score. Computed tomography (CT) scan of the abdomen revealed severe intrahepatic biliary duct dilatation due to TIPS compression of the central common hepatic duct. Endoscopic retrograde cholangiopancreatography (ERCP) was performed with placement of plastic stent in the common bile duct for decompression. Repeat abdominal CT demonstrated improved right-sided biliary duct dilation with ongoing severe left biliary duct dilation. IR-guided percutaneous biliary drain placement was performed, with improvement of hyperbilirubinemia. The patient was discharged from the hospital with continued liver transplant evaluation planned outpatient.
Discussion: Presented is a rare complication of TIPS placement leading to biliary obstruction and worsening acute on chronic liver failure. Although this patient was at risk of having alcohol-associated hepatitis given her ongoing alcohol use, it is important to consider TIPS complications as a cause for worsening liver failure. Although the most common cause of increasing bilirubin after TIPS is liver failure from hepatic ischemia, obstruction of the biliary duct system by the TIPS must be considered and remain on the differential.
Disclosures:
Yash Hegde, MD1, Dana A. Ley, MD2, Adnan Said, MD, MS2, Prasad Dalvie, MD1, Mark Benson, MD1, Deepak V. Gopal, MD, FACG2. P3019 - Biliary Obstruction from Transjugular Intrahepatic Portosystemic Shunt Mimicking Alcohol-Associated Hepatitis - A Rare Complication, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Wisconsin School of Medicine and Public Health, Madison, WI; 2University of Wisconsin Hospitals and Clinics, Madison, WI
Introduction: Transjugular intrahepatic portosystemic shunt (TIPS) is a procedure used to decrease portal hypertension. The two most common clinical indications for TIPS include secondary prevention of variceal hemorrhage and refractory ascites. Biliary complications, most commonly biliary-shunt fistula formation, remain relatively rare. Biliary obstruction secondary to TIPS placement is a rare complication, with few cases reported in the literature.
Case Description/Methods: A 52-year-old female with alcohol use disorder and decompensated alcohol-related cirrhosis, complicated by portal hypertension with ascites and recurrent episodes of variceal hemorrhage despite variceal band ligation, presented with hematemesis. Her blood alcohol level was significantly elevated at 300 mg/dL. Esophagogastroduodenoscopy (EGD) demonstrated multiple gastric varices secondary to portal hypertension, not actively bleeding. She underwent TIPS placement with improvement in hepatic venous pressure gradient from 15 to 8 mm Hg. Post-TIPS, her Model for End-stage Liver Disease (MELD) score increased which was suspected to be secondary to alcohol-associated hepatitis or TIPS induced ischemic hepatitis. She was started on N-acetylcysteine and steroids, which were ineffective, as demonstrated by continued increase in MELD score. Computed tomography (CT) scan of the abdomen revealed severe intrahepatic biliary duct dilatation due to TIPS compression of the central common hepatic duct. Endoscopic retrograde cholangiopancreatography (ERCP) was performed with placement of plastic stent in the common bile duct for decompression. Repeat abdominal CT demonstrated improved right-sided biliary duct dilation with ongoing severe left biliary duct dilation. IR-guided percutaneous biliary drain placement was performed, with improvement of hyperbilirubinemia. The patient was discharged from the hospital with continued liver transplant evaluation planned outpatient.
Discussion: Presented is a rare complication of TIPS placement leading to biliary obstruction and worsening acute on chronic liver failure. Although this patient was at risk of having alcohol-associated hepatitis given her ongoing alcohol use, it is important to consider TIPS complications as a cause for worsening liver failure. Although the most common cause of increasing bilirubin after TIPS is liver failure from hepatic ischemia, obstruction of the biliary duct system by the TIPS must be considered and remain on the differential.
Figure: ERCP showing common hepatic duct obstruction secondary to TIPS stent with intrahepatic duct dilation and subsequent stent placement (Image A and B). As liver function tests did not improve, interventional radiology performed percutaneous transhepatic cholangiogram and placed biliary drain (Image C).
Disclosures:
Yash Hegde indicated no relevant financial relationships.
Dana Ley indicated no relevant financial relationships.
Adnan Said indicated no relevant financial relationships.
Prasad Dalvie indicated no relevant financial relationships.
Mark Benson indicated no relevant financial relationships.
Deepak Gopal indicated no relevant financial relationships.
Yash Hegde, MD1, Dana A. Ley, MD2, Adnan Said, MD, MS2, Prasad Dalvie, MD1, Mark Benson, MD1, Deepak V. Gopal, MD, FACG2. P3019 - Biliary Obstruction from Transjugular Intrahepatic Portosystemic Shunt Mimicking Alcohol-Associated Hepatitis - A Rare Complication, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

