Monday Poster Session
Category: Liver
P3025 - Not Quite the Same: Comparative Cases of Drug-Induced Autoimmune and Autoimmune-Like Hepatitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Benjamin Cardenas, MD
Walter Reed National Military Medical Center
Bethesda, MD
Presenting Author(s)
Benjamin Cardenas, MD, Azfar S. Syed, DO, MBA, Maria Sjogren, MD, MPH
Walter Reed National Military Medical Center, Bethesda, MD
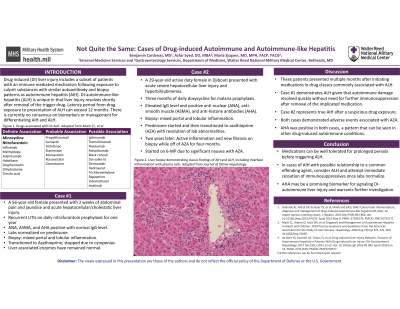
Introduction: Drug induced (DI) liver injury includes a subset of patients with an immune mediated mechanism following exposure to culprit substances. These can be further differentiated into DI-autoimmune hepatitis (AIH) and DI-autoimmune-like hepatitis (ALH) with the predominant difference being that ALH does not require lifelong immunosuppression. There is currently no consensus on biomarkers or management for differentiating these diagnoses.
Case Description/Methods: An active duty 29-year-old female stationed in Djibouti presented with fatigue, nausea, and jaundice in the setting of three months of daily doxycycline use for malaria prophylaxis. She was found to have acute severe hepatocellular liver injury and hyperbilirubinemia. Testing was significant for elevated IgG level and positive anti-nuclear (ANA), anti-smooth muscle (ASMA), and anti-histone antibodies (AHA). The patient was medically evacuated to a tertiary care center where she was diagnosed with AIH and was started on daily prednisone. Biopsy demonstrated mixed portal and lobular inflammation. Steroids were tapered and azathioprine was initiated followed by resolution of lab abnormalities. Two years later, follow-up biopsy while off immunosuppression for four months demonstrated continued grade two inflammation with stage one fibrosis. The decision was made to continue indefinite immunosuppression.
A 56-year-old female with recurrent urinary tract infections on daily nitrofurantoin prophylaxis for one year presented with abdominal pain and jaundice and was found to have acute hepatocellular and cholestatic liver injury. ANA, ASMA, and AHA tests were positive with normal IgG level. Daily prednisone was started, and liver associated enzymes normalized. Biopsy demonstrated mixed portal and lobular inflammation, as well. Azathioprine was initiated, and over 10 months, steroids were tapered. Two months after steroids were stopped, azathioprine was stopped due to cytopenias. Liver associated enzymes have remained normal since.
Discussion: Medications can unmask AIH in predisposed individuals. However, a subset of these individuals likely have ALH, and would benefit from a trial of immunosuppressant cessation. AHA positivity may be a promising biomarker for future investigation for differentiating ALH from AIH, with the former also lacking IgG elevation. It is important that clinicians accurately differentiate between these two similar conditions due to the significant morbidity associated with long term immunosuppressant use.
Disclosures:
Benjamin Cardenas, MD, Azfar S. Syed, DO, MBA, Maria Sjogren, MD, MPH. P3025 - Not Quite the Same: Comparative Cases of Drug-Induced Autoimmune and Autoimmune-Like Hepatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Drug induced (DI) liver injury includes a subset of patients with an immune mediated mechanism following exposure to culprit substances. These can be further differentiated into DI-autoimmune hepatitis (AIH) and DI-autoimmune-like hepatitis (ALH) with the predominant difference being that ALH does not require lifelong immunosuppression. There is currently no consensus on biomarkers or management for differentiating these diagnoses.
Case Description/Methods: An active duty 29-year-old female stationed in Djibouti presented with fatigue, nausea, and jaundice in the setting of three months of daily doxycycline use for malaria prophylaxis. She was found to have acute severe hepatocellular liver injury and hyperbilirubinemia. Testing was significant for elevated IgG level and positive anti-nuclear (ANA), anti-smooth muscle (ASMA), and anti-histone antibodies (AHA). The patient was medically evacuated to a tertiary care center where she was diagnosed with AIH and was started on daily prednisone. Biopsy demonstrated mixed portal and lobular inflammation. Steroids were tapered and azathioprine was initiated followed by resolution of lab abnormalities. Two years later, follow-up biopsy while off immunosuppression for four months demonstrated continued grade two inflammation with stage one fibrosis. The decision was made to continue indefinite immunosuppression.
A 56-year-old female with recurrent urinary tract infections on daily nitrofurantoin prophylaxis for one year presented with abdominal pain and jaundice and was found to have acute hepatocellular and cholestatic liver injury. ANA, ASMA, and AHA tests were positive with normal IgG level. Daily prednisone was started, and liver associated enzymes normalized. Biopsy demonstrated mixed portal and lobular inflammation, as well. Azathioprine was initiated, and over 10 months, steroids were tapered. Two months after steroids were stopped, azathioprine was stopped due to cytopenias. Liver associated enzymes have remained normal since.
Discussion: Medications can unmask AIH in predisposed individuals. However, a subset of these individuals likely have ALH, and would benefit from a trial of immunosuppressant cessation. AHA positivity may be a promising biomarker for future investigation for differentiating ALH from AIH, with the former also lacking IgG elevation. It is important that clinicians accurately differentiate between these two similar conditions due to the significant morbidity associated with long term immunosuppressant use.
Disclosures:
Benjamin Cardenas indicated no relevant financial relationships.
Azfar Syed indicated no relevant financial relationships.
Maria Sjogren indicated no relevant financial relationships.
Benjamin Cardenas, MD, Azfar S. Syed, DO, MBA, Maria Sjogren, MD, MPH. P3025 - Not Quite the Same: Comparative Cases of Drug-Induced Autoimmune and Autoimmune-Like Hepatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
