Monday Poster Session
Category: Liver
P3033 - Seronegative Autoimmune Hepatitis: A Challenging Diagnosis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Shany M. Quevedo, MD
Aventura Hospital
Miami, FL
Presenting Author(s)
Shany M. Quevedo, MD1, Deannys Batista, MD1, Jose Rodriguez Castro, MD2, Nathan Ramasamy, MD2
1Aventura Hospital, Miami, FL; 2Aventura Hospital, Aventura, FL
Introduction: Autoimmune hepatitis (AIH) is an inflammatory liver disease that may present as a progressive disease, acute liver failure or cirrhosis and is usually associated with the presence of autoantibodies. Antibody positive AIH is known as seropositive AIH (spAIH). Conversely, seronegative autoimmune hepatitis (snAIH) is of similar presentation, pathology and disease trajectory; however, given snAIH lacks positive serology, it constitutes a challenging diagnosis [1,2]. We present a case of a 63-year-old female who presented with nonspecific symptoms and strikingly high transaminases and was found to have seronegative AIH.
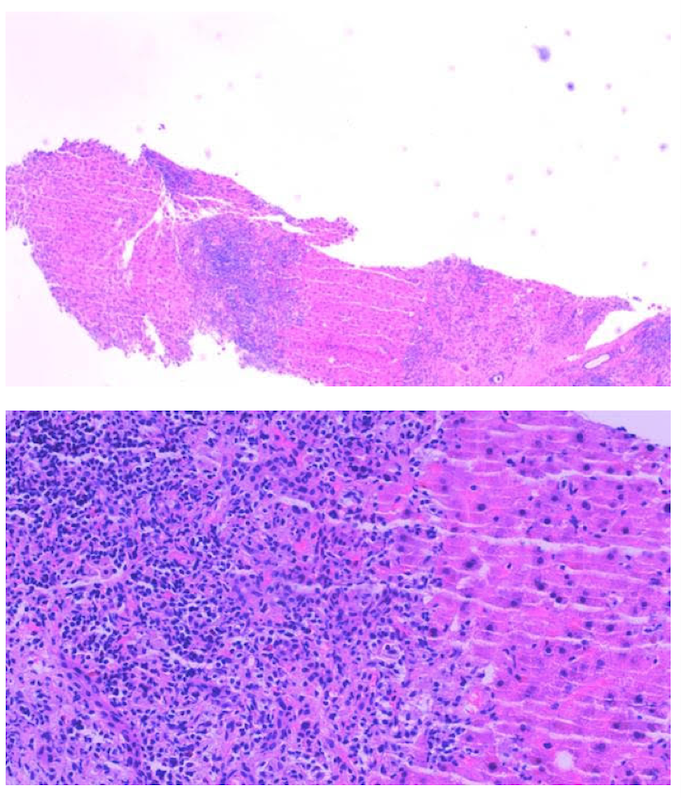
Case Description/Methods: Our patient is a 63-year-old female without significant past medical history who presented with complaints of malaise, fatigue, and substantially elevated transaminases. The patient denied personal or family history of liver disease, as well as an extensive social history. Initial labs revealed AST 1562, ALT 2014, alkaline phosphatase 353, INR of 1.3 and MELD-Na score of 18. The patient was mentating well and exhibited mild scleral icterus and jaundice. Abdominal imaging revealed a subcentimeter simple liver cyst. Workup for Wilson’s disease, Celiac’s disease, additional autoimmune diseases, viral etiologies, DILI, ischemic hepatitis, and Budd Chiari were unrevealing. Anti-mitochondrial antibody, ASMA, LKMI1 and immunoglobulins were negative. Liver biopsy showed portal inflammation with marked inflammatory infiltrates composed predominantly of lymphocytes with interface activity and patchy periportal hepatocellular and focal bridging dropout, suggestive of AIH. The revised original score for AIH revealed probable diagnosis. After prompt initiation of methylprednisolone, the patient displayed marked biochemical and clinical improvement, confirming our diagnosis.
Discussion: AIH has a wide spectrum of presentation, ranging from asymptomatic to fulminant disease. Most cases are ANA or ASMA antibody positive and carry elevated immunoglobulin levels; however, 10% of cases have negative serologic workup [1]. Given its indolent but potentially fatal nature, it is important to consider the diagnosis in cases with negative serology [1,2,3]. As described in the study by Sherigar, et. al, the use of scoring systems for AIH can aid in the diagnosis, especially if suspecting snAIH [3]. Therefore, it is imperative that one remains with a high degree of suspicion for AIH, for a liver biopsy must be obtained, allowing for prompt diagnosis and early steroid therapy.
Disclosures:
Shany M. Quevedo, MD1, Deannys Batista, MD1, Jose Rodriguez Castro, MD2, Nathan Ramasamy, MD2. P3033 - Seronegative Autoimmune Hepatitis: A Challenging Diagnosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Aventura Hospital, Miami, FL; 2Aventura Hospital, Aventura, FL
Introduction: Autoimmune hepatitis (AIH) is an inflammatory liver disease that may present as a progressive disease, acute liver failure or cirrhosis and is usually associated with the presence of autoantibodies. Antibody positive AIH is known as seropositive AIH (spAIH). Conversely, seronegative autoimmune hepatitis (snAIH) is of similar presentation, pathology and disease trajectory; however, given snAIH lacks positive serology, it constitutes a challenging diagnosis [1,2]. We present a case of a 63-year-old female who presented with nonspecific symptoms and strikingly high transaminases and was found to have seronegative AIH.
Case Description/Methods: Our patient is a 63-year-old female without significant past medical history who presented with complaints of malaise, fatigue, and substantially elevated transaminases. The patient denied personal or family history of liver disease, as well as an extensive social history. Initial labs revealed AST 1562, ALT 2014, alkaline phosphatase 353, INR of 1.3 and MELD-Na score of 18. The patient was mentating well and exhibited mild scleral icterus and jaundice. Abdominal imaging revealed a subcentimeter simple liver cyst. Workup for Wilson’s disease, Celiac’s disease, additional autoimmune diseases, viral etiologies, DILI, ischemic hepatitis, and Budd Chiari were unrevealing. Anti-mitochondrial antibody, ASMA, LKMI1 and immunoglobulins were negative. Liver biopsy showed portal inflammation with marked inflammatory infiltrates composed predominantly of lymphocytes with interface activity and patchy periportal hepatocellular and focal bridging dropout, suggestive of AIH. The revised original score for AIH revealed probable diagnosis. After prompt initiation of methylprednisolone, the patient displayed marked biochemical and clinical improvement, confirming our diagnosis.
Discussion: AIH has a wide spectrum of presentation, ranging from asymptomatic to fulminant disease. Most cases are ANA or ASMA antibody positive and carry elevated immunoglobulin levels; however, 10% of cases have negative serologic workup [1]. Given its indolent but potentially fatal nature, it is important to consider the diagnosis in cases with negative serology [1,2,3]. As described in the study by Sherigar, et. al, the use of scoring systems for AIH can aid in the diagnosis, especially if suspecting snAIH [3]. Therefore, it is imperative that one remains with a high degree of suspicion for AIH, for a liver biopsy must be obtained, allowing for prompt diagnosis and early steroid therapy.
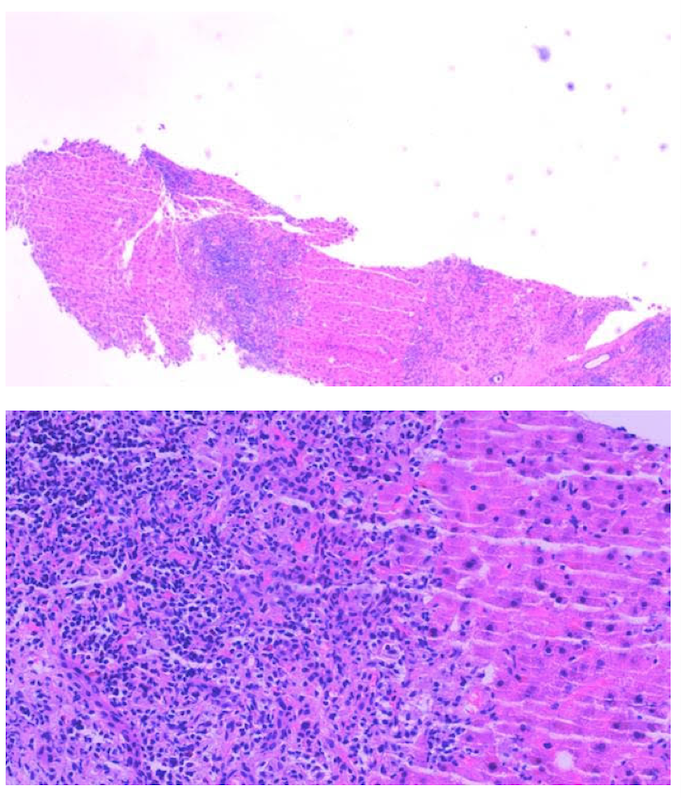
Figure: Inflammatory infiltrates predominantly of lymphocytes with interface activity and patchy periportal hepatocellular and focal bridging dropout
Disclosures:
Shany Quevedo indicated no relevant financial relationships.
Deannys Batista indicated no relevant financial relationships.
Jose Rodriguez Castro indicated no relevant financial relationships.
Nathan Ramasamy indicated no relevant financial relationships.
Shany M. Quevedo, MD1, Deannys Batista, MD1, Jose Rodriguez Castro, MD2, Nathan Ramasamy, MD2. P3033 - Seronegative Autoimmune Hepatitis: A Challenging Diagnosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
