Monday Poster Session
Category: Liver
P2939 - Comparison of Interventions for Pyogenic Liver Abscess at the National Level
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Faris Shweikeh, MD
Cleveland Clinic Akron General
Akron, OH
Presenting Author(s)
Faris Shweikeh, MD1, Yaritza Torres, BS2, Naga Venkata Rama Krishna Vura, MD3, Neha Sharma, MD4, Anthony Leung, DO5, Amandeep Singh, MD1, Anamay N. Sharma, MD6
1Cleveland Clinic Akron General, Akron, OH; 2Northeast Ohio Medical University, Rootstown, OH; 3University of Texas Health San Antonio, San Antonio, TX; 4University of Texas Health Science Center, San Antonio, TX; 5Cleveland Clinic, Akron, OH; 6Case Western Reserve University School of Medicine, Cleveland, OH
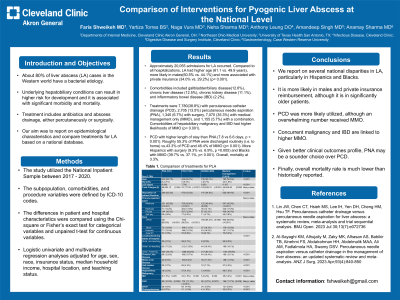
Introduction: About 80% of liver abscess (LA) cases in the Western world have a bacterial etiology. Underlying hepatobiliary conditions can result in higher risk for development and it is associated with significant morbidity and mortality. Treatment includes antibiotics and abscess drainage, either percutaneously or surgically. Our aim was to report on epidemiological characteristics and compare treatments for LA based on a national database.
Methods: The study utilized the National Inpatient Sample between 2017 - 2020. The subpopulation, comorbidities, and procedure variables were defined by ICD-10 codes. The differences in patient and hospital characteristics were compared using the Chi-square or Fisher’s exact test for categorical variables and unpaired t-test for continuous variables. Logistic univariate and multivariate regression analyses adjusted for age, sex, race, insurance status, median household income, hospital location, and teaching status.
Results: Approximately 20,055 admissions for LA occurred. Compared to all hospitalizations, LA had higher age (61.1 vs. 49.9 years), more likely in males (60.5% vs. 44.1%) and more associated with private insurance (34.0% vs. 29.2%) (p< 0.001). Comorbidities included gallbladder/biliary disease (12.6%), chronic liver disease (12.5%), chronic kidney disease (11.1%), and inflammatory bowel disease (IBD) (2.2%). Treatments were 7,780 (38.8%) with percutaneous catheter drainage (PCD), 2,705 (13.5%) percutaneous needle aspiration (PNA), 1,345 (6.7%) with surgery, 7,070 (35.3%) with medical management only (MMO), and 1,155 (5.7%) with a combination. Comorbidities of hepatobiliary malignancy and IBD had higher likelihoods of MMO (p< 0.001). PCD with higher length of stay than PNA (7.8 vs 6.6 days, p < 0.001). Roughly 55.3% of PNA were discharged routinely (i.e. to home) vs.43.3% of PCD and 46.4% of MMO (p< 0.001). More Hispanics with surgery (9.3% vs. 6.9%, p =0.005) and Blacks with MMO (39.7% vs. 37.1%, p< 0.001). Overall, mortality at 3.3%.
Discussion: We report on several national disparities in LA, particularly in Hispanics and Blacks. It is more likely in males and private insurance reimbursement, although it is in significantly older patients. PCD was more likely utilized, although an overwhelming number received MMO. Concurrent malignancy and IBD are linked to higher MMO. Given better clinical outcomes profile, PNA may be a sounder choice over PCD. Finally, mortality rate is much lower than historically reported.
Disclosures:
Faris Shweikeh, MD1, Yaritza Torres, BS2, Naga Venkata Rama Krishna Vura, MD3, Neha Sharma, MD4, Anthony Leung, DO5, Amandeep Singh, MD1, Anamay N. Sharma, MD6. P2939 - Comparison of Interventions for Pyogenic Liver Abscess at the National Level, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic Akron General, Akron, OH; 2Northeast Ohio Medical University, Rootstown, OH; 3University of Texas Health San Antonio, San Antonio, TX; 4University of Texas Health Science Center, San Antonio, TX; 5Cleveland Clinic, Akron, OH; 6Case Western Reserve University School of Medicine, Cleveland, OH
Introduction: About 80% of liver abscess (LA) cases in the Western world have a bacterial etiology. Underlying hepatobiliary conditions can result in higher risk for development and it is associated with significant morbidity and mortality. Treatment includes antibiotics and abscess drainage, either percutaneously or surgically. Our aim was to report on epidemiological characteristics and compare treatments for LA based on a national database.
Methods: The study utilized the National Inpatient Sample between 2017 - 2020. The subpopulation, comorbidities, and procedure variables were defined by ICD-10 codes. The differences in patient and hospital characteristics were compared using the Chi-square or Fisher’s exact test for categorical variables and unpaired t-test for continuous variables. Logistic univariate and multivariate regression analyses adjusted for age, sex, race, insurance status, median household income, hospital location, and teaching status.
Results: Approximately 20,055 admissions for LA occurred. Compared to all hospitalizations, LA had higher age (61.1 vs. 49.9 years), more likely in males (60.5% vs. 44.1%) and more associated with private insurance (34.0% vs. 29.2%) (p< 0.001). Comorbidities included gallbladder/biliary disease (12.6%), chronic liver disease (12.5%), chronic kidney disease (11.1%), and inflammatory bowel disease (IBD) (2.2%). Treatments were 7,780 (38.8%) with percutaneous catheter drainage (PCD), 2,705 (13.5%) percutaneous needle aspiration (PNA), 1,345 (6.7%) with surgery, 7,070 (35.3%) with medical management only (MMO), and 1,155 (5.7%) with a combination. Comorbidities of hepatobiliary malignancy and IBD had higher likelihoods of MMO (p< 0.001). PCD with higher length of stay than PNA (7.8 vs 6.6 days, p < 0.001). Roughly 55.3% of PNA were discharged routinely (i.e. to home) vs.43.3% of PCD and 46.4% of MMO (p< 0.001). More Hispanics with surgery (9.3% vs. 6.9%, p =0.005) and Blacks with MMO (39.7% vs. 37.1%, p< 0.001). Overall, mortality at 3.3%.
Discussion: We report on several national disparities in LA, particularly in Hispanics and Blacks. It is more likely in males and private insurance reimbursement, although it is in significantly older patients. PCD was more likely utilized, although an overwhelming number received MMO. Concurrent malignancy and IBD are linked to higher MMO. Given better clinical outcomes profile, PNA may be a sounder choice over PCD. Finally, mortality rate is much lower than historically reported.
Disclosures:
Faris Shweikeh indicated no relevant financial relationships.
Yaritza Torres indicated no relevant financial relationships.
Naga Venkata Rama Krishna Vura indicated no relevant financial relationships.
Neha Sharma indicated no relevant financial relationships.
Anthony Leung indicated no relevant financial relationships.
Amandeep Singh indicated no relevant financial relationships.
Anamay Sharma indicated no relevant financial relationships.
Faris Shweikeh, MD1, Yaritza Torres, BS2, Naga Venkata Rama Krishna Vura, MD3, Neha Sharma, MD4, Anthony Leung, DO5, Amandeep Singh, MD1, Anamay N. Sharma, MD6. P2939 - Comparison of Interventions for Pyogenic Liver Abscess at the National Level, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
