Monday Poster Session
Category: Liver
P2941 - Disparities and Clinical Associations Related to Portal Vein Thrombosis in Hospitalized Patients With Cirrhosis: A Nationwide Analysis (NIS 1998-2015)
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- DP
David Putt, DO, MBA
Ascension Providence Hospital
Southfield, MI
Presenting Author(s)
David Putt, DO, MBA, George Felemegos, MD, Saif Affas, MD
Ascension Providence Hospital, Southfield, MI
Introduction: Portal vein thrombosis (PVT) is a significant and potentially serious complication observed in patients with liver cirrhosis (LC) during hospitalization. This study is aimed to elucidate discrepancies and clinical associations of PVT in LC patients through analysis of the National Inpatient Sample (NIS).
Methods: This study was performed using the 1998-2015 NIS to assess disparities among patients with cirrhosis and concurrent PVT as well as the relationship between PVT and cirrhosis-related outcomes. Using chi-square analysis, statistical significance was defined as a P value < .05.
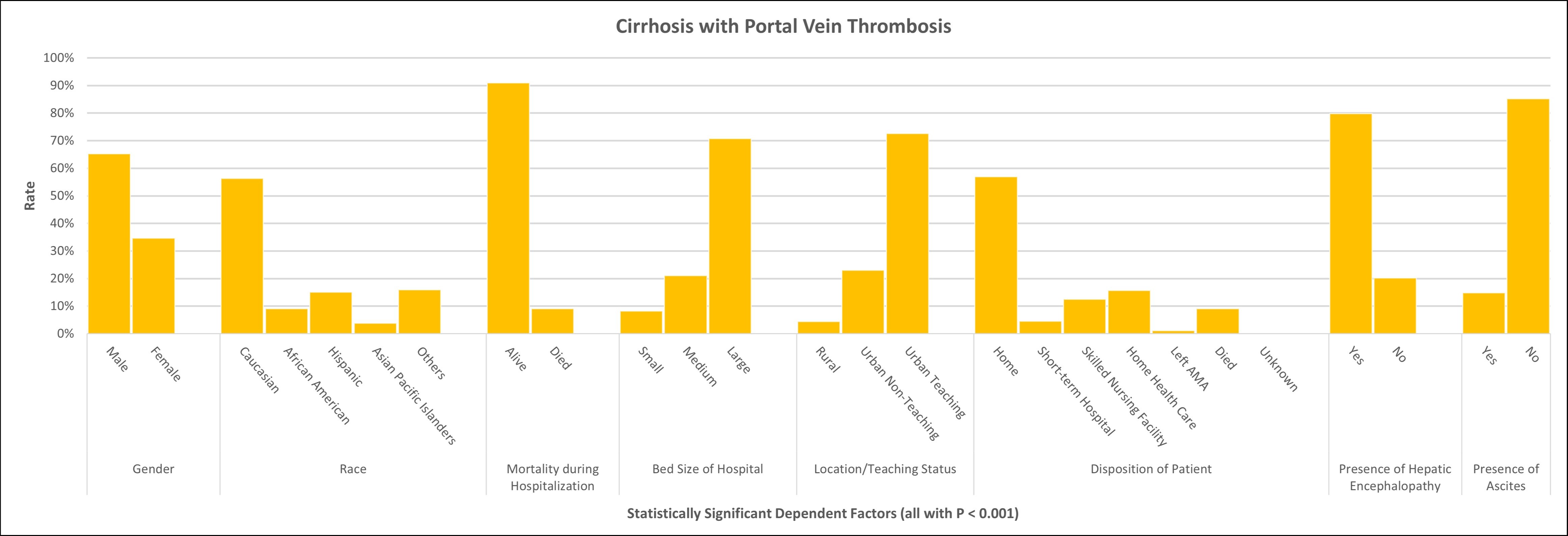
Results: Of the 7,670,271 patients admitted with PVT in the setting of cirrhosis from the 1998-2015 NIS, the prevalence of PVT was more prominent in males (n=65.3%) compared to females (n=34.7%) in those with cirrhosis (P< .001). Caucasian patients had the highest occurrence of PVT (n=56.3%). The in-hospital mortality rate for patients admitted with cirrhosis and PVT was 9.1%. Large-size hospitals had the highest reported PVT in patients with cirrhosis (n=70.8%) compared to medium-size hospitals (n=21.0%) and small-size hospitals (n=8.2%) (P< .001). Urban teaching hospitals were the most common location for treatment (n=72.6%) with urban non-teaching (n=23.0%) and rural hospitals (n=4.4%) having much lower such admissions (P< .001). The majority of the included patients went home from the hospital (n=56.9%). On univariate analysis, patients who had a diagnosis of both cirrhosis and PVT had higher proportions of hepatic encephalopathy (20.2% vs 17.5%; P< .001) as well as higher proportions of ascites (14.8% vs 14.3%; P < .001). Patients with cirrhosis and PVT also incurred a greater average length of stay and greater total hospital charges.
Discussion: This study leveraged data from the NIS, revealing notable disparities, with males and Caucasians exhibiting a higher prevalence of PVT. The 9.1% in-hospital mortality rate emphasizes the clinical significance of this comorbidity. Large hospitals, particularly urban teaching hospitals, reported higher PVT prevalence, suggesting potential healthcare access and resource influences. Patients with both cirrhosis and PVT experienced increased complications, emphasizing the synergistic impact of these conditions. While age at admission did not significantly differ, the observed disparities highlight the need for further exploration of genetic, environmental, and healthcare access factors influencing PVT development in this population.
Disclosures:
David Putt, DO, MBA, George Felemegos, MD, Saif Affas, MD. P2941 - Disparities and Clinical Associations Related to Portal Vein Thrombosis in Hospitalized Patients With Cirrhosis: A Nationwide Analysis (NIS 1998-2015), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Ascension Providence Hospital, Southfield, MI
Introduction: Portal vein thrombosis (PVT) is a significant and potentially serious complication observed in patients with liver cirrhosis (LC) during hospitalization. This study is aimed to elucidate discrepancies and clinical associations of PVT in LC patients through analysis of the National Inpatient Sample (NIS).
Methods: This study was performed using the 1998-2015 NIS to assess disparities among patients with cirrhosis and concurrent PVT as well as the relationship between PVT and cirrhosis-related outcomes. Using chi-square analysis, statistical significance was defined as a P value < .05.
Results: Of the 7,670,271 patients admitted with PVT in the setting of cirrhosis from the 1998-2015 NIS, the prevalence of PVT was more prominent in males (n=65.3%) compared to females (n=34.7%) in those with cirrhosis (P< .001). Caucasian patients had the highest occurrence of PVT (n=56.3%). The in-hospital mortality rate for patients admitted with cirrhosis and PVT was 9.1%. Large-size hospitals had the highest reported PVT in patients with cirrhosis (n=70.8%) compared to medium-size hospitals (n=21.0%) and small-size hospitals (n=8.2%) (P< .001). Urban teaching hospitals were the most common location for treatment (n=72.6%) with urban non-teaching (n=23.0%) and rural hospitals (n=4.4%) having much lower such admissions (P< .001). The majority of the included patients went home from the hospital (n=56.9%). On univariate analysis, patients who had a diagnosis of both cirrhosis and PVT had higher proportions of hepatic encephalopathy (20.2% vs 17.5%; P< .001) as well as higher proportions of ascites (14.8% vs 14.3%; P < .001). Patients with cirrhosis and PVT also incurred a greater average length of stay and greater total hospital charges.
Discussion: This study leveraged data from the NIS, revealing notable disparities, with males and Caucasians exhibiting a higher prevalence of PVT. The 9.1% in-hospital mortality rate emphasizes the clinical significance of this comorbidity. Large hospitals, particularly urban teaching hospitals, reported higher PVT prevalence, suggesting potential healthcare access and resource influences. Patients with both cirrhosis and PVT experienced increased complications, emphasizing the synergistic impact of these conditions. While age at admission did not significantly differ, the observed disparities highlight the need for further exploration of genetic, environmental, and healthcare access factors influencing PVT development in this population.
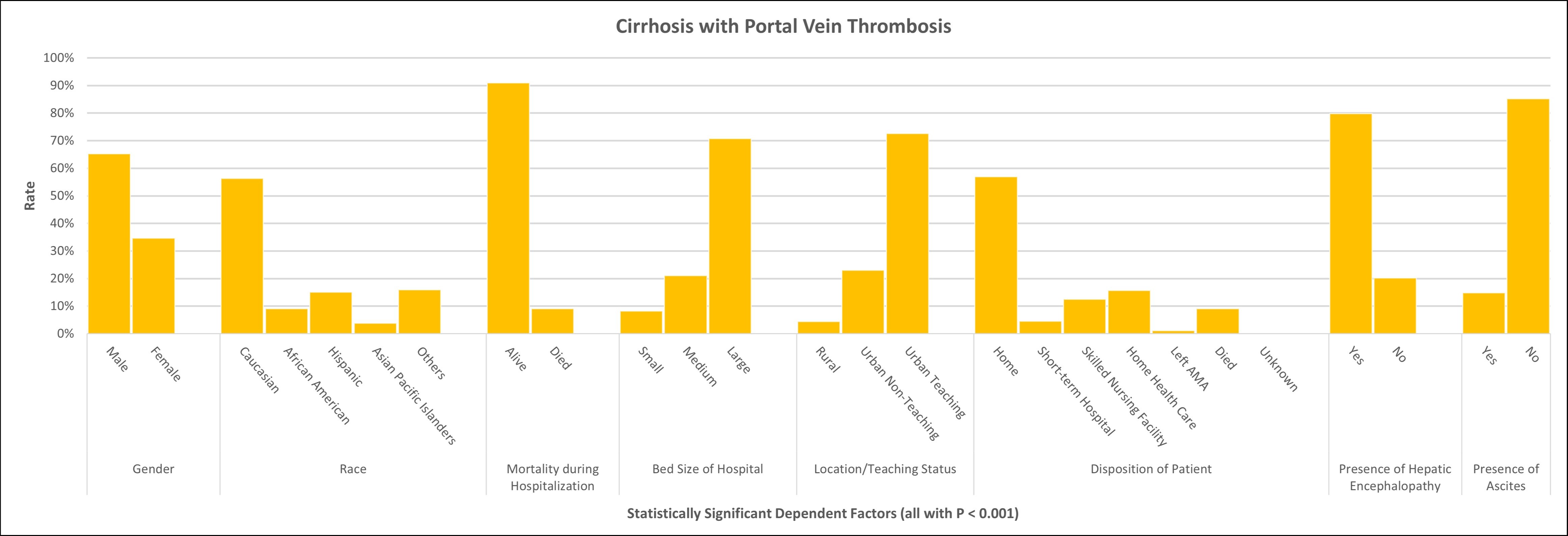
Figure: Here are the statistically significant disparities and clinical associations related to portal vein thrombosis in hospitalized patients with cirrhosis from the National Inpatient Sample database (NIS 1998-2015).
Disclosures:
David Putt indicated no relevant financial relationships.
George Felemegos indicated no relevant financial relationships.
Saif Affas indicated no relevant financial relationships.
David Putt, DO, MBA, George Felemegos, MD, Saif Affas, MD. P2941 - Disparities and Clinical Associations Related to Portal Vein Thrombosis in Hospitalized Patients With Cirrhosis: A Nationwide Analysis (NIS 1998-2015), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
