Monday Poster Session
Category: Liver
P2953 - Role of Pre-Operative TIPS in Patients Undergoing Surgery
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Mitchell L Shiffman, MD
Liver Institute of Virginia, Bon Secours Health System
Richmond, VA
Presenting Author(s)
Award: Presidential Poster Award
Mitchell L Shiffman, MD
Liver Institute of Virginia, Bon Secours Health System, Richmond, VA
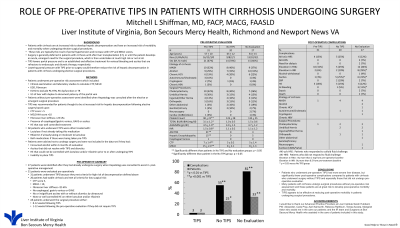
Introduction: Patients with cirrhosis are at increased risk to develop hepatic decompensation and have an increased risk of morbidity and mortality when undergoing elective surgical procedures. These risks are typically the result of portal hypertension and increased CTP and MELD scores. Placement of a TIPS lowers portal pressure and is an effective treatment for refractory variceal bleeding and ascites. Several small case reports have suggested that TIPS could possibly lower morbidity and mortality in patients undergoing elective surgery. This retrospective analysis compared patients with cirrhosis who underwent pre-operative TIPS to patients who underwent surgery without TIPS at our hospital over an 11 year period.
Methods: Patients with cirrhosis were either referred to Hepatology for pre-operative risk assessment or were seen as an in-patient after undergoing a surgical procedure. TIPS was recommended for patients who were thought to be at increased risk for hepatic decompensation following surgery based upon the following: CTP >5, MELD-NA >10, history of esophageal/gastric varices, GAVE or ascites. All patients who underwent TPS were either started on lactulose, rifaximin if already taking lactulose or continued on lactulose and xifaxan if already on these medications. Pre-operative laboratory data and post-operative complications and mortality were assessed.
Results: 51 patients were evaluated pre-operatively. TIPS was recommended and performed in 31 patients. Another 25 patients were not known to have cirrhosis and underwent surgery without pre-operative evaluation. The mean age for all patients was 56 yrs, 66% were male. The most common etiology for cirrhosis was MASH (35%), ETOH (32%), HCV 20%. The surgical procedures included cholecystectomy (31%), umbilical hernia (21%), inguinal or other hernia (12%), orthopedic surgery (15%), other abdominal surgery (11%), GU surgery (7%) and CABG (3%). Pre-operative and post-operative outcomes are summarized (TABLE).
Discussion: Patients who underwent pre-operative TIPS had more severe liver disease but fewer post-operative complications compared to patients with cirrhosis who did not undergo pre-operative TIPS. Many patients with unrecognized cirrhosis undergo surgical procedures and these patients may at greatest risk to develop post-operative morbidity and mortality. TIPS appears to be effective at reducing post-operative morbidity in patients undergoing surgery.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mitchell L Shiffman, MD. P2953 - Role of Pre-Operative TIPS in Patients Undergoing Surgery, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mitchell L Shiffman, MD
Liver Institute of Virginia, Bon Secours Health System, Richmond, VA
Introduction: Patients with cirrhosis are at increased risk to develop hepatic decompensation and have an increased risk of morbidity and mortality when undergoing elective surgical procedures. These risks are typically the result of portal hypertension and increased CTP and MELD scores. Placement of a TIPS lowers portal pressure and is an effective treatment for refractory variceal bleeding and ascites. Several small case reports have suggested that TIPS could possibly lower morbidity and mortality in patients undergoing elective surgery. This retrospective analysis compared patients with cirrhosis who underwent pre-operative TIPS to patients who underwent surgery without TIPS at our hospital over an 11 year period.
Methods: Patients with cirrhosis were either referred to Hepatology for pre-operative risk assessment or were seen as an in-patient after undergoing a surgical procedure. TIPS was recommended for patients who were thought to be at increased risk for hepatic decompensation following surgery based upon the following: CTP >5, MELD-NA >10, history of esophageal/gastric varices, GAVE or ascites. All patients who underwent TPS were either started on lactulose, rifaximin if already taking lactulose or continued on lactulose and xifaxan if already on these medications. Pre-operative laboratory data and post-operative complications and mortality were assessed.
Results: 51 patients were evaluated pre-operatively. TIPS was recommended and performed in 31 patients. Another 25 patients were not known to have cirrhosis and underwent surgery without pre-operative evaluation. The mean age for all patients was 56 yrs, 66% were male. The most common etiology for cirrhosis was MASH (35%), ETOH (32%), HCV 20%. The surgical procedures included cholecystectomy (31%), umbilical hernia (21%), inguinal or other hernia (12%), orthopedic surgery (15%), other abdominal surgery (11%), GU surgery (7%) and CABG (3%). Pre-operative and post-operative outcomes are summarized (TABLE).
Discussion: Patients who underwent pre-operative TIPS had more severe liver disease but fewer post-operative complications compared to patients with cirrhosis who did not undergo pre-operative TIPS. Many patients with unrecognized cirrhosis undergo surgical procedures and these patients may at greatest risk to develop post-operative morbidity and mortality. TIPS appears to be effective at reducing post-operative morbidity in patients undergoing surgery.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mitchell L Shiffman: 89Bio – Grant/Research Support. Akero – Grant/Research Support. Altimmune – Grant/Research Support. CymaBay – Advisory Committee/Board Member, Grant/Research Support. Durect – Grant/Research Support. Galectin – Grant/Research Support. Genentech – Grant/Research Support, Speakers Bureau. Gilead – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Hamni – Grant/Research Support. HepQuant – Advisory Committee/Board Member, Grant/Research Support. HighTide – Grant/Research Support. Intercept – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Intra-Sana – Advisor or Review Panel Member, Speakers Bureau. Ipsen – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Madrigal – Grant/Research Support, Speakers Bureau. Mallinckodt – Speakers Bureau. Mirum – Advisory Committee/Board Member, Grant/Research Support. Novo Nordisk – Grant/Research Support. Pliant – Grant/Research Support. Salix – Grant/Research Support. Viking Therapeutics – Grant/Research Support.
Mitchell L Shiffman, MD. P2953 - Role of Pre-Operative TIPS in Patients Undergoing Surgery, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

