Monday Poster Session
Category: Liver
P2856 - The Comparative Risk of Upper Gastrointestinal Bleeding With Carvedilol Versus Propranolol in Patients With Liver Cirrhosis: A Retrospective Study
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Abdellatif Ismail, MD
University of Maryland Medical Center
Baltimore, MD
Presenting Author(s)
Abdellatif Ismail, MD1, Mahmoud Y. Madi, MD2, Wing-kin Syn, MD, PhD3
1University of Maryland Medical Center, Baltimore, MD; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3Saint Louis University School of Medicine, St. Louis, MO
Introduction: The use of non-selective beta blockers (NSBB) in patients with liver cirrhosis to decrease the risk of esophageal variceal bleeding and other portal hypertension complications has been well-established and evidence-based. However, comparative studies between various NSBB have been sparsely reported in the literature.
Methods: We conducted a propensity score matched retrospective cohort study using the TriNetX platform, which is a global research database based on electronic health records. Adult patients with a history of liver cirrhosis between October 2015 and December 2023 were included. The cohort was divided into patients on propranolol and patients on carvedilol. The observation period was 30 days to 5 years after starting the index NSBB. The primary outcome was the development of upper gastrointestinal bleeding (UGIB) within the observation period. The secondary outcomes included the development of hepatic encephalopathy (HE), ascites and mortality within the observation period. One-to-one propensity score matching (PSM) was performed to balance the demographics, cardiovascular, renal and hematologic disorders, baseline biochemistry, and medications between the two cohorts. After PSM, the risk of each outcome was calculated and expressed as odds ratios (OR) with 95% confidence intervals (CI). Two-sided P values < 0.05 were considered statistically significant.
Results: Before PSM, there were 37,321 patients in the propranolol group and 46,073 patients in the carvedilol group. After PSM, 26,620 patients were analyzed in each cohort.
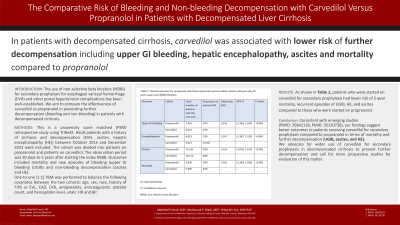
A total of 7,301 patients (27%) in the propranolol group developed UGIB compared to 6,211 patients (23%) in the carvedilol group, OR: 1.24, P-value < 0.001. HE developed in 4,013 patients (15%) in the propranolol group compared to 3,317 patients (12.5%) in the carvedilol group, OR: 1.24, P-value < 0.001. A total of 11,413 patients (43%) in the propranolol group developed new-onset or worsening ascites compared to 10,716 patients (40%) in the carvedilol group, OR: 1.11, P-value < 0.001, Table 1. Furthermore, patients who were started on carvedilol had lower mortality within the observation period (n=5,965, 22%) compared to the propranolol group (n=6,920, 26%), OR 1.21, P-value < 0.001.
Discussion: In patients with liver cirrhosis, carvedilol was associated with lower risk of developing upper GI bleeding, hepatic encephalopathy, ascites and mortality compared to propranolol after matching for confounding factors.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abdellatif Ismail, MD1, Mahmoud Y. Madi, MD2, Wing-kin Syn, MD, PhD3. P2856 - The Comparative Risk of Upper Gastrointestinal Bleeding With Carvedilol Versus Propranolol in Patients With Liver Cirrhosis: A Retrospective Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Maryland Medical Center, Baltimore, MD; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3Saint Louis University School of Medicine, St. Louis, MO
Introduction: The use of non-selective beta blockers (NSBB) in patients with liver cirrhosis to decrease the risk of esophageal variceal bleeding and other portal hypertension complications has been well-established and evidence-based. However, comparative studies between various NSBB have been sparsely reported in the literature.
Methods: We conducted a propensity score matched retrospective cohort study using the TriNetX platform, which is a global research database based on electronic health records. Adult patients with a history of liver cirrhosis between October 2015 and December 2023 were included. The cohort was divided into patients on propranolol and patients on carvedilol. The observation period was 30 days to 5 years after starting the index NSBB. The primary outcome was the development of upper gastrointestinal bleeding (UGIB) within the observation period. The secondary outcomes included the development of hepatic encephalopathy (HE), ascites and mortality within the observation period. One-to-one propensity score matching (PSM) was performed to balance the demographics, cardiovascular, renal and hematologic disorders, baseline biochemistry, and medications between the two cohorts. After PSM, the risk of each outcome was calculated and expressed as odds ratios (OR) with 95% confidence intervals (CI). Two-sided P values < 0.05 were considered statistically significant.
Results: Before PSM, there were 37,321 patients in the propranolol group and 46,073 patients in the carvedilol group. After PSM, 26,620 patients were analyzed in each cohort.
A total of 7,301 patients (27%) in the propranolol group developed UGIB compared to 6,211 patients (23%) in the carvedilol group, OR: 1.24, P-value < 0.001. HE developed in 4,013 patients (15%) in the propranolol group compared to 3,317 patients (12.5%) in the carvedilol group, OR: 1.24, P-value < 0.001. A total of 11,413 patients (43%) in the propranolol group developed new-onset or worsening ascites compared to 10,716 patients (40%) in the carvedilol group, OR: 1.11, P-value < 0.001, Table 1. Furthermore, patients who were started on carvedilol had lower mortality within the observation period (n=5,965, 22%) compared to the propranolol group (n=6,920, 26%), OR 1.21, P-value < 0.001.
Discussion: In patients with liver cirrhosis, carvedilol was associated with lower risk of developing upper GI bleeding, hepatic encephalopathy, ascites and mortality compared to propranolol after matching for confounding factors.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abdellatif Ismail indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Wing-kin Syn: Merck – Consultant. Zydus – Grant/Research Support.
Abdellatif Ismail, MD1, Mahmoud Y. Madi, MD2, Wing-kin Syn, MD, PhD3. P2856 - The Comparative Risk of Upper Gastrointestinal Bleeding With Carvedilol Versus Propranolol in Patients With Liver Cirrhosis: A Retrospective Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

