Monday Poster Session
Category: Liver
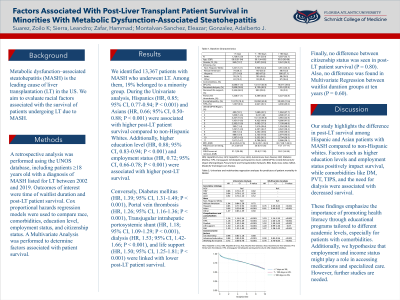
P2868 - Factors Associated With Post-Liver Transplant Patient Survival in Minorities With Metabolic Dysfunction-Associated Steatohepatitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Zoilo K. Suarez, MD
Florida Atlantic University, Charles E. Schmidt College of Medicine
Boca Raton, FL
Presenting Author(s)
Zoilo K. Suarez, MD1, Leandro Sierra, MD2, Hammad Zafar, MD3, Eleazar Enrique. Montalvan-Sanchez, MD4, Adalberto Gonzalez, MD3
1Florida Atlantic University, Charles E. Schmidt College of Medicine, Boca Raton, FL; 2Cleveland Clinic Foundation, Cleveland, OH; 3Cleveland Clinic Florida, Weston, FL; 4Yale Digestive Diseases, New Haven, CT
Introduction: Metabolic dysfunction–associated steatohepatitis (MASH) is the leading cause of liver transplantation (LT) in the US. We aim to evaluate racial factors associated with the survival of patients undergoing LT due to MASH.
Methods: A retrospective analysis was performed using the UNOS database, including patients ≥18 years old with a diagnosis of MASH listed for LT between 2002 and 2019. Outcomes of interest were time of waitlist duration and post-LT patient survival. Cox proportional hazards regression models were used to compare race, comorbidities, education level, employment status, and citizenship status. A Multivariate Analysis was performed to determine factors associated with patient survival.
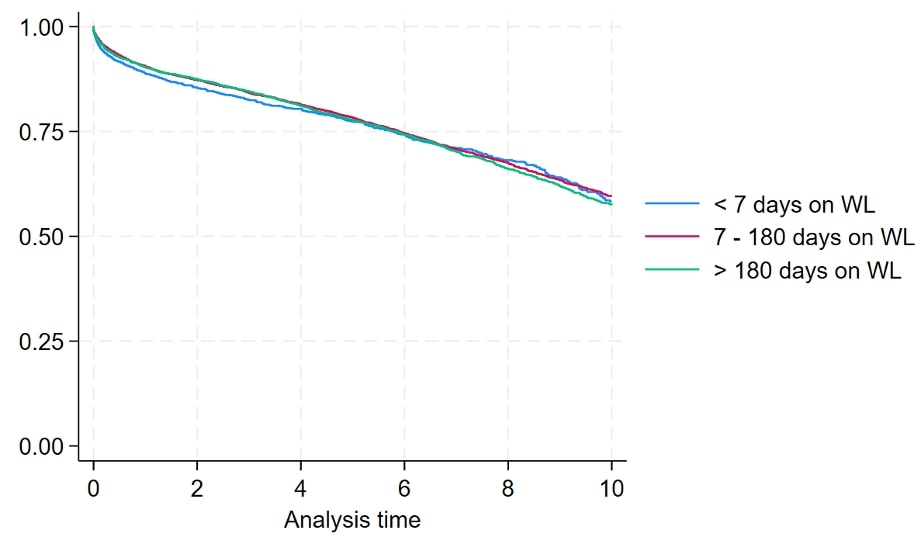
Results: We identified 13,367 patients with MASH who underwent LT. Among them, 19% belonged to a minority group. During the Univariate analysis, Hispanics (HR, 0.85; 95% CI, 0.77-0.94; P < 0.001) and Asians (HR, 0.66; 95% CI, 0.50-0.88; P < 0.001) were associated with higher post-LT patient survival compared to non-Hispanic Whites. Additionally, higher education level (HR, 0.88; 95% CI, 0.83-0.94; P < 0.001) and employment status (HR, 0.72; 95% CI, 0.66-0.78; P < 0.001) were associated with higher post-LT survival. Conversely, Diabetes mellitus (HR, 1.39; 95% CI, 1.31-1.49; P < 0.001), Portal vein thrombosis (HR, 1.26; 95% CI, 1.16-1.36; P < 0.001), Transjugular intrahepatic portosystemic shunt (HR, 1.18; 95% CI, 1.09-1.29; P < 0.001), dialysis (HR, 1.53; 95% CI, 1.42-1.66; P < 0.001), and life support (HR, 1.50; 95% CI, 1.25-1.81; P < 0.001) were linked with lower post-LT patient survival. Finally, no difference between citizenship status was seen in post-LT patient survival (P = 0.80). Also, no difference was found in Multivariate Regression between waitlist duration groups at ten years (P = 0.60).
Discussion: Our study highlights the difference in post-LT survival among Hispanic and Asian patients with MASH compared to non-Hispanic whites. Factors such as higher education levels and employment status positively impact survival, while comorbidities like DM, PVT, TIPS, and the need for dialysis were associated with decreased survival. These findings emphasize the importance of promoting health literacy through educational programs tailored to different academic levels, especially for patients with comorbidities. Additionally, we hypothesize that employment and income status might play a role in accessing medications and specialized care. However, further studies are needed.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Zoilo K. Suarez, MD1, Leandro Sierra, MD2, Hammad Zafar, MD3, Eleazar Enrique. Montalvan-Sanchez, MD4, Adalberto Gonzalez, MD3. P2868 - Factors Associated With Post-Liver Transplant Patient Survival in Minorities With Metabolic Dysfunction-Associated Steatohepatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Florida Atlantic University, Charles E. Schmidt College of Medicine, Boca Raton, FL; 2Cleveland Clinic Foundation, Cleveland, OH; 3Cleveland Clinic Florida, Weston, FL; 4Yale Digestive Diseases, New Haven, CT
Introduction: Metabolic dysfunction–associated steatohepatitis (MASH) is the leading cause of liver transplantation (LT) in the US. We aim to evaluate racial factors associated with the survival of patients undergoing LT due to MASH.
Methods: A retrospective analysis was performed using the UNOS database, including patients ≥18 years old with a diagnosis of MASH listed for LT between 2002 and 2019. Outcomes of interest were time of waitlist duration and post-LT patient survival. Cox proportional hazards regression models were used to compare race, comorbidities, education level, employment status, and citizenship status. A Multivariate Analysis was performed to determine factors associated with patient survival.
Results: We identified 13,367 patients with MASH who underwent LT. Among them, 19% belonged to a minority group. During the Univariate analysis, Hispanics (HR, 0.85; 95% CI, 0.77-0.94; P < 0.001) and Asians (HR, 0.66; 95% CI, 0.50-0.88; P < 0.001) were associated with higher post-LT patient survival compared to non-Hispanic Whites. Additionally, higher education level (HR, 0.88; 95% CI, 0.83-0.94; P < 0.001) and employment status (HR, 0.72; 95% CI, 0.66-0.78; P < 0.001) were associated with higher post-LT survival. Conversely, Diabetes mellitus (HR, 1.39; 95% CI, 1.31-1.49; P < 0.001), Portal vein thrombosis (HR, 1.26; 95% CI, 1.16-1.36; P < 0.001), Transjugular intrahepatic portosystemic shunt (HR, 1.18; 95% CI, 1.09-1.29; P < 0.001), dialysis (HR, 1.53; 95% CI, 1.42-1.66; P < 0.001), and life support (HR, 1.50; 95% CI, 1.25-1.81; P < 0.001) were linked with lower post-LT patient survival. Finally, no difference between citizenship status was seen in post-LT patient survival (P = 0.80). Also, no difference was found in Multivariate Regression between waitlist duration groups at ten years (P = 0.60).
Discussion: Our study highlights the difference in post-LT survival among Hispanic and Asian patients with MASH compared to non-Hispanic whites. Factors such as higher education levels and employment status positively impact survival, while comorbidities like DM, PVT, TIPS, and the need for dialysis were associated with decreased survival. These findings emphasize the importance of promoting health literacy through educational programs tailored to different academic levels, especially for patients with comorbidities. Additionally, we hypothesize that employment and income status might play a role in accessing medications and specialized care. However, further studies are needed.
Figure: Figure 1. Kaplan-Meyer survival curve for waitlist duration in patients with MASH (P=0.60)
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Zoilo Suarez indicated no relevant financial relationships.
Leandro Sierra indicated no relevant financial relationships.
Hammad Zafar indicated no relevant financial relationships.
Eleazar Montalvan-Sanchez indicated no relevant financial relationships.
Adalberto Gonzalez indicated no relevant financial relationships.
Zoilo K. Suarez, MD1, Leandro Sierra, MD2, Hammad Zafar, MD3, Eleazar Enrique. Montalvan-Sanchez, MD4, Adalberto Gonzalez, MD3. P2868 - Factors Associated With Post-Liver Transplant Patient Survival in Minorities With Metabolic Dysfunction-Associated Steatohepatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

