Monday Poster Session
Category: Interventional Endoscopy
P2796 - Angiocatheter and Miniature Biopsy Forceps to Facilitate Suture Delivery and Closure as a Novel Technique for Enterocutaneous Fistula Closure
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Neev Mehta, MD
Lahey Hospital and Medical Center
Burlington, MA
Presenting Author(s)
Neev Mehta, MD1, Neethi Dasu, DO2, Khaldoon Khirfan, MD2, Haider Rahman, MD1, Mena Bakhit, MD1
1Lahey Hospital and Medical Center, Burlington, MA; 2Beth Israel Lahey Health, Burlington, MA
Introduction: Percutaneous endoscopic gastrostomy (PEG) tube has become one of the preferred modalities for enteral nutrition. Complications from PEG include buried bumper syndrome, infection, colonic perforation, bleeding, tube dislodgment/malfunction, and persistent gastrocutaneous fistula (GCF). We present a case of an entero-cutaneous fistula in a patient with a chronic PEG, requiring endo-cutaneous suturing using an angiocatheter and miniature biopsy forceps. Due to significant esophageal stricture, other endoscopic modalities for suturing of fistula were not feasible.
Case Description/Methods: An 85-year-old male with multiple comorbidities, including oropharyngeal cancer status post resection and radiation, hypopharynx with dysphagia, and PEG tube dependent for enteral nutrition, had presented with a chronic complaint of leakage from previous PEG tube site. Options were considered to perform upper esophageal sphincter dilation due to a history of radiation, followed by endoscopic suturing using an endoscopic suturing device or by over-the-scope clip technique.
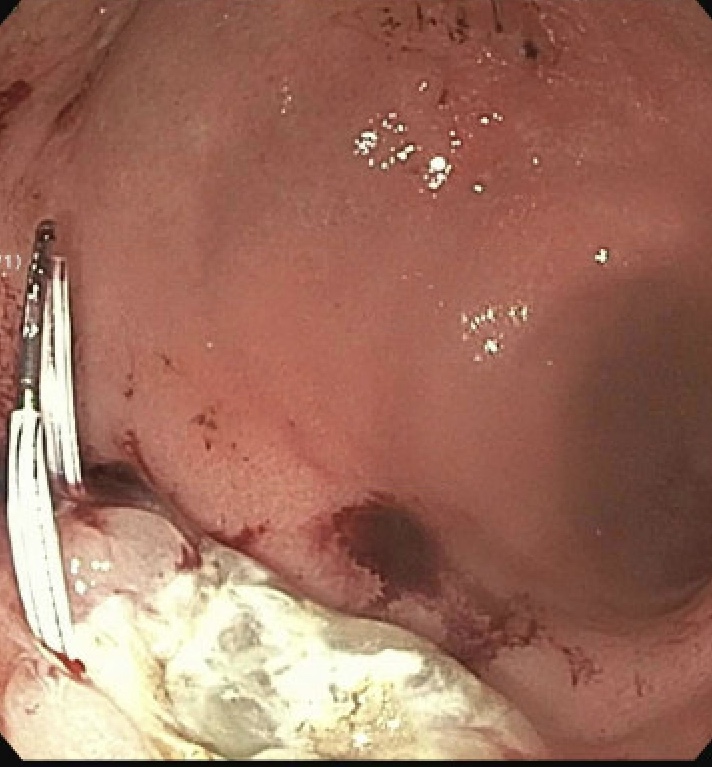
At the time of endoscopy, extensive scarring in the hypopharynx was seen, with resistance near the gastroesophageal junction due to circumferential scarring. Balloon dilation up to 15 mm was performed, ensuring no deep muscle injury. A 1 mm fistula was noted in the gastric antrum. The endoscopic suturing device turned out to be too large to pass through the esophageal sphincter due to prior radiation to the area. Under endoscopic guidance, two 16 gauge angiocatheters were advanced into the gastric lumen, one cranial, and one caudal to the fistula tract. 2-0 nylon suture was advanced through 1 angiocath, externalized using miniature biopsy forceps through the other angiocatheter. The Angiocatheters were removed over sutures, and the loop was tied. This process was repeated two more times, providing full fistula closure.
Discussion: Persistent GCF is a rare but well-known adverse event that occurs after the removal of a PEG tube when spontaneous closure fails. Endoscopic therapies for management include over-the-scope clips, endoscopic suturing, and biosynthetic glue.
In prior endoscopic suturing techniques, the suture loop is externalized through the GCF mouth or tract, limiting motion. In this case, we describe using a novel method that employs miniature biopsy forceps to externalize the suture to ensure maneuverability and adequate fistula closure. This technique can be an effective modality when conventional modalities cannot be implemented.
Disclosures:
Neev Mehta, MD1, Neethi Dasu, DO2, Khaldoon Khirfan, MD2, Haider Rahman, MD1, Mena Bakhit, MD1. P2796 - Angiocatheter and Miniature Biopsy Forceps to Facilitate Suture Delivery and Closure as a Novel Technique for Enterocutaneous Fistula Closure, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Lahey Hospital and Medical Center, Burlington, MA; 2Beth Israel Lahey Health, Burlington, MA
Introduction: Percutaneous endoscopic gastrostomy (PEG) tube has become one of the preferred modalities for enteral nutrition. Complications from PEG include buried bumper syndrome, infection, colonic perforation, bleeding, tube dislodgment/malfunction, and persistent gastrocutaneous fistula (GCF). We present a case of an entero-cutaneous fistula in a patient with a chronic PEG, requiring endo-cutaneous suturing using an angiocatheter and miniature biopsy forceps. Due to significant esophageal stricture, other endoscopic modalities for suturing of fistula were not feasible.
Case Description/Methods: An 85-year-old male with multiple comorbidities, including oropharyngeal cancer status post resection and radiation, hypopharynx with dysphagia, and PEG tube dependent for enteral nutrition, had presented with a chronic complaint of leakage from previous PEG tube site. Options were considered to perform upper esophageal sphincter dilation due to a history of radiation, followed by endoscopic suturing using an endoscopic suturing device or by over-the-scope clip technique.
At the time of endoscopy, extensive scarring in the hypopharynx was seen, with resistance near the gastroesophageal junction due to circumferential scarring. Balloon dilation up to 15 mm was performed, ensuring no deep muscle injury. A 1 mm fistula was noted in the gastric antrum. The endoscopic suturing device turned out to be too large to pass through the esophageal sphincter due to prior radiation to the area. Under endoscopic guidance, two 16 gauge angiocatheters were advanced into the gastric lumen, one cranial, and one caudal to the fistula tract. 2-0 nylon suture was advanced through 1 angiocath, externalized using miniature biopsy forceps through the other angiocatheter. The Angiocatheters were removed over sutures, and the loop was tied. This process was repeated two more times, providing full fistula closure.
Discussion: Persistent GCF is a rare but well-known adverse event that occurs after the removal of a PEG tube when spontaneous closure fails. Endoscopic therapies for management include over-the-scope clips, endoscopic suturing, and biosynthetic glue.
In prior endoscopic suturing techniques, the suture loop is externalized through the GCF mouth or tract, limiting motion. In this case, we describe using a novel method that employs miniature biopsy forceps to externalize the suture to ensure maneuverability and adequate fistula closure. This technique can be an effective modality when conventional modalities cannot be implemented.
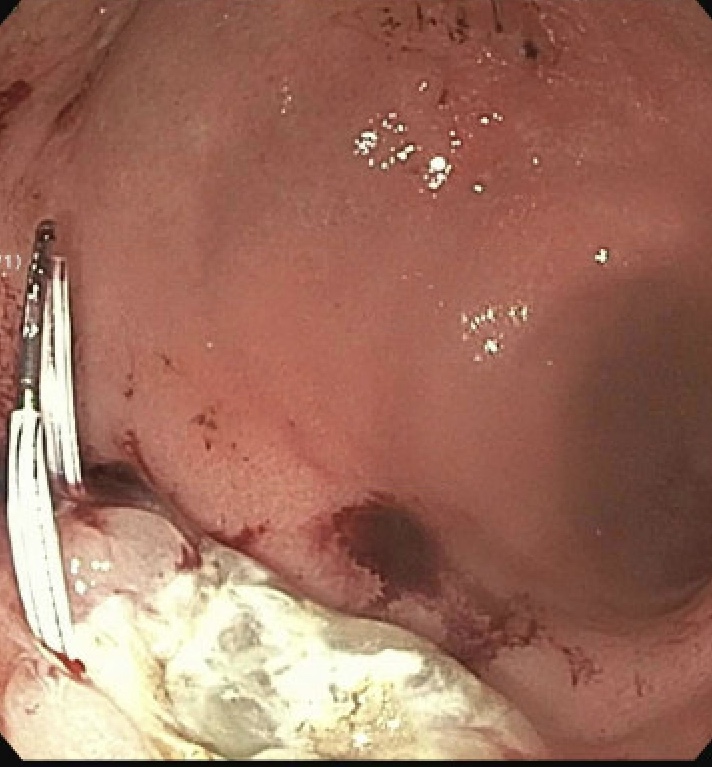
Figure: Angiocatheter for suturing
Disclosures:
Neev Mehta indicated no relevant financial relationships.
Neethi Dasu indicated no relevant financial relationships.
Khaldoon Khirfan indicated no relevant financial relationships.
Haider Rahman indicated no relevant financial relationships.
Mena Bakhit indicated no relevant financial relationships.
Neev Mehta, MD1, Neethi Dasu, DO2, Khaldoon Khirfan, MD2, Haider Rahman, MD1, Mena Bakhit, MD1. P2796 - Angiocatheter and Miniature Biopsy Forceps to Facilitate Suture Delivery and Closure as a Novel Technique for Enterocutaneous Fistula Closure, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
