Monday Poster Session
Category: Interventional Endoscopy
P2800 - Bile Duct Obstruction Caused by Portal Vein Cavernous Transformation
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Hong T. Lin, MD
The Ohio State University Wexner Medical Center
Columbus, OH
Presenting Author(s)
Award: Presidential Poster Award
Hong T. Lin, MD, Somashekar G Krishna, MD, Erica Park, MD
The Ohio State University Wexner Medical Center, Columbus, OH
Introduction: Cavernous transformation of the portal vein (CTPV) is characterized by dilation of the portal vein and the development of tortuous collateral vessels. Rare in adults, CTPV typically results from portal vein thrombosis or obstruction. It regularly mimics liver cirrhosis, causing portal hypertensive symptoms such as ascites, varices, and obstructive biliopathy due to compressive mass effects. Secondary vascular changes may also alter hepatic morphology. Anticoagulation treatment is usually ineffective due to complete venous obstruction and treatment is often procedural.
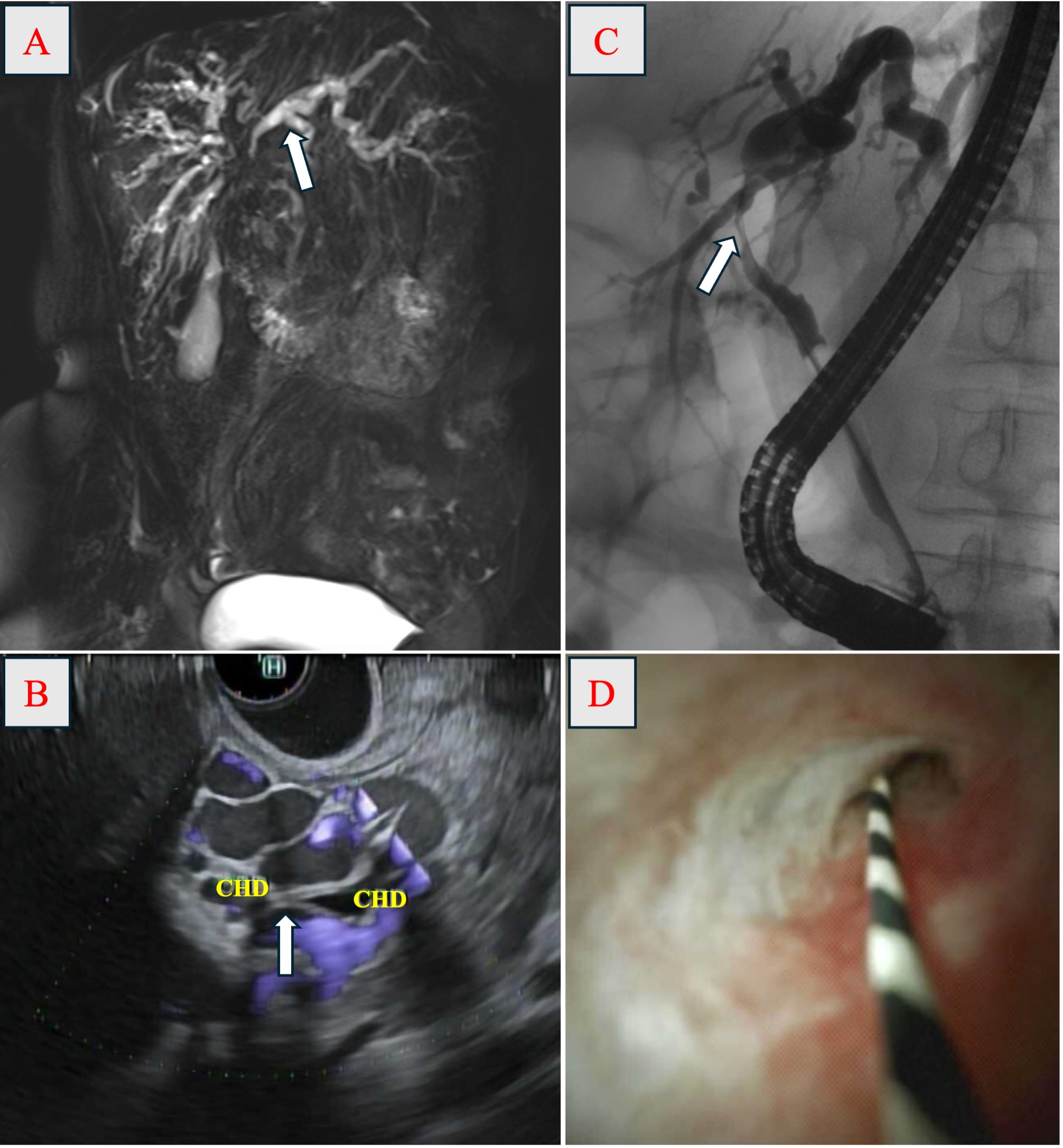
Case Description/Methods: A 65-year-old woman with human immunodeficiency virus (HIV) infection presented with a 2-week history of progressive weight loss, malaise, and dysphagia. Laboratory tests revealed a cholestatic pattern of liver injury, with alkaline phosphatase of 423 U/L and total bilirubin of 2.6 mg/dL. Magnetic resonance imaging demonstrated moderate intrahepatic biliary ductal dilation and an ill-defined 3 cm lesion at the porta hepatis with delayed enhancement (Panel A). The surrounding lymph nodes, gallbladder, and pancreas appeared normal. Endoscopic ultrasound (EUS) revealed extensive collateral veins that compress on the common hepatic duct (CHD), leading to upstream intrahepatic ductal dilation (Panel B). Endoscopic retrograde cholangiopancreatography (ERCP) confirmed a 24 mm biliary stricture in the CHD, consistent with EUS findings (Panel C). Cholangioscopy showed a moderately narrowed CHD lumen with normal mucosa and no evidence of tumor or inflammation (Panel D). Placement of a biliary stent resulted in improvement of the patient’s liver enzyme levels.
Discussion: CTPV often mimics common diseases and causes nonspecific symptoms such as fatigue, anorexia, and weight loss. It is usually diagnosed late during evaluation for variceal bleeding, splenomegaly, or refractory ascites. Although hepatic cirrhosis is a significant risk factor, CTPV may occur independently or in conjunction with other coagulopathies, such as those found in HIV infection. This case underscores a rare, benign etiology of portal cavernoma cholangiopathy, resulting in bile duct compression and obstruction. Cholangioscopy can help rule out intraductal inflammatory or malignant processes. Endoscopic biliary stenting, the modified transjugular intrahepatic portosystemic shunt (mTIPS) procedure, or portal vein stenting may be considered to address biliopathy and the underlying CTPV.
Disclosures:
Hong T. Lin, MD, Somashekar G Krishna, MD, Erica Park, MD. P2800 - Bile Duct Obstruction Caused by Portal Vein Cavernous Transformation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Hong T. Lin, MD, Somashekar G Krishna, MD, Erica Park, MD
The Ohio State University Wexner Medical Center, Columbus, OH
Introduction: Cavernous transformation of the portal vein (CTPV) is characterized by dilation of the portal vein and the development of tortuous collateral vessels. Rare in adults, CTPV typically results from portal vein thrombosis or obstruction. It regularly mimics liver cirrhosis, causing portal hypertensive symptoms such as ascites, varices, and obstructive biliopathy due to compressive mass effects. Secondary vascular changes may also alter hepatic morphology. Anticoagulation treatment is usually ineffective due to complete venous obstruction and treatment is often procedural.
Case Description/Methods: A 65-year-old woman with human immunodeficiency virus (HIV) infection presented with a 2-week history of progressive weight loss, malaise, and dysphagia. Laboratory tests revealed a cholestatic pattern of liver injury, with alkaline phosphatase of 423 U/L and total bilirubin of 2.6 mg/dL. Magnetic resonance imaging demonstrated moderate intrahepatic biliary ductal dilation and an ill-defined 3 cm lesion at the porta hepatis with delayed enhancement (Panel A). The surrounding lymph nodes, gallbladder, and pancreas appeared normal. Endoscopic ultrasound (EUS) revealed extensive collateral veins that compress on the common hepatic duct (CHD), leading to upstream intrahepatic ductal dilation (Panel B). Endoscopic retrograde cholangiopancreatography (ERCP) confirmed a 24 mm biliary stricture in the CHD, consistent with EUS findings (Panel C). Cholangioscopy showed a moderately narrowed CHD lumen with normal mucosa and no evidence of tumor or inflammation (Panel D). Placement of a biliary stent resulted in improvement of the patient’s liver enzyme levels.
Discussion: CTPV often mimics common diseases and causes nonspecific symptoms such as fatigue, anorexia, and weight loss. It is usually diagnosed late during evaluation for variceal bleeding, splenomegaly, or refractory ascites. Although hepatic cirrhosis is a significant risk factor, CTPV may occur independently or in conjunction with other coagulopathies, such as those found in HIV infection. This case underscores a rare, benign etiology of portal cavernoma cholangiopathy, resulting in bile duct compression and obstruction. Cholangioscopy can help rule out intraductal inflammatory or malignant processes. Endoscopic biliary stenting, the modified transjugular intrahepatic portosystemic shunt (mTIPS) procedure, or portal vein stenting may be considered to address biliopathy and the underlying CTPV.
Figure: Image 1: (A) Intrahepatic biliary dilation (arrow) upstream of the porta hepatis lesion, (B) common hepatic duct (CHD) compression (arrow) by collateral veins on EUS, (C) CTPV with CHD stricture, and (D) CHD stricture with otherwise normal lumen on cholangioscopy.
Disclosures:
Hong Lin indicated no relevant financial relationships.
Somashekar G Krishna: Boston Scientific – Consultant. Mauna Kea Technologies, and TaeWoong Medical USA – Grant/Research Support. TaeWoong Medical USA – Grant/Research Support.
Erica Park indicated no relevant financial relationships.
Hong T. Lin, MD, Somashekar G Krishna, MD, Erica Park, MD. P2800 - Bile Duct Obstruction Caused by Portal Vein Cavernous Transformation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

