Monday Poster Session
Category: Interventional Endoscopy
P2806 - Partial Endoscopic Sleeve Gastroplasty for Management of Gastric Perforation During Intragastric Balloon Placement
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- RS
Ryan L. Santos, DO
San Antonio Uniformed Services Health Education Consortium
San Antonio, TX
Presenting Author(s)
Award: Presidential Poster Award
Ryan L. Santos, DO1, John G. Quiles, MD2, Jerome C. Edelson, MD3
1San Antonio Uniformed Services Health Education Consortium, San Antonio, TX; 2Brooke Army Medical Center, San Antonio, TX; 3Brooke Army Medical Center, Fort Sam Houston, TX
Introduction: Placement of intragastric balloons (IGB) for weight loss, while generally safe and well tolerated, can lead to rare complications such as gastric perforation. If recognized at the time of placement, the perforation can be managed endoscopically. Here, we present a case of a gastric perforation during IGB placement and its management through endoscopic suturing with conversion to partial Endoscopic Sleeve Gastroplasty (ESG).
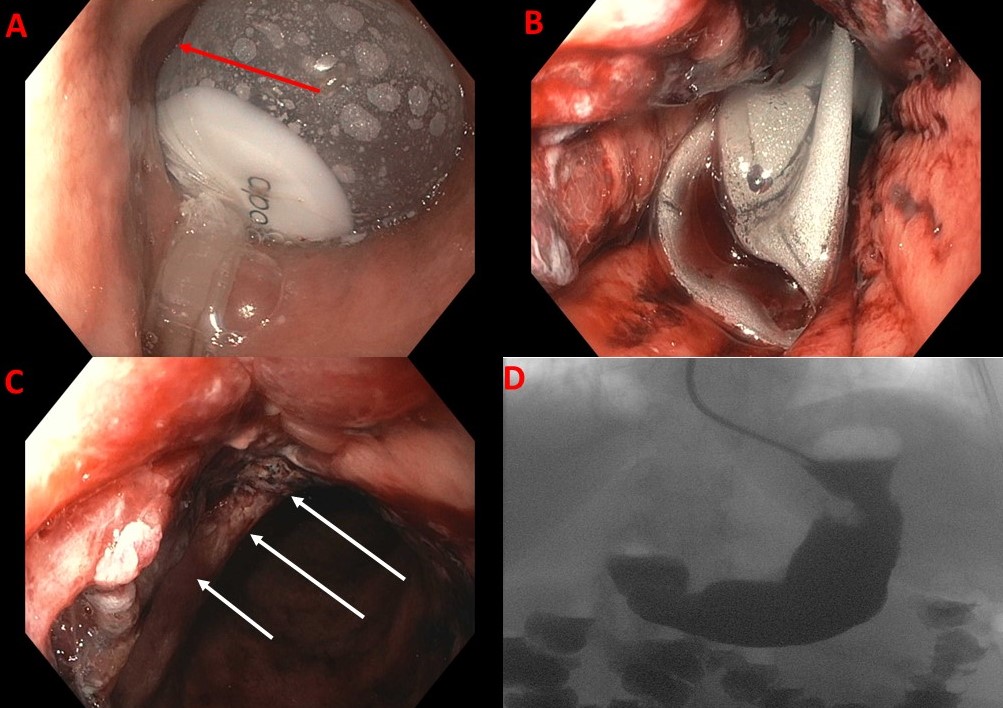
Case Description/Methods: A 63-year-old female with a BMI of 35 underwent IGB placement following unsuccessful attempts with lifestyle modifications, phentermine and orlistat. During endoscopy, the IGB was advanced into the stomach and sequentially inflated with 600ml of saline. Immediately following inflation, retroflexion in the body demonstrated a mucosal rent behind the balloon prompting intubation prior to IGB removal (Image A, arrow; Image B). Upon reentering the stomach, a 3 cm full-thickness perforation was identified along the anterior wall. IV antibiotics were given and a surgeon was consulted intraoperatively with plans made for surgery if endoscopic closure was not successful. A dual-channel therapeutic endoscope with suturing device was then introduced and 2 sutures were placed in a running fashion to close the defect (Image C, arrows). Contrast injection into the gastric lumen revealed a residual leak and an additional suture was added for reinforcement in a running fashion akin to ESG. Repeat injection showed no leak. She was admitted for observation.
The following day, she underwent an upper GI series which did not show any extravasation (Image D). Her diet was advanced and she was transitioned to a bariatric diet for six weeks. At two months, she had lost 18 lbs. without further complications.
Discussion: IGB placement is a safe, well-established, and well-tolerated weight loss procedure, but it carries risks inherent to endoscopic interventions. Despite thorough patient selection, including negative Helicobacter pylori status and absence of structural abnormalities or prior gastric/bariatric surgeries, IGB placement resulted in gastric perforation. Prompt recognition, antibiotic administration, surgical consultation, and closure using an endoscopic suture device in a running fashion, akin to ESG, led to favorable outcomes including continued weight loss.
Disclosures:
Ryan L. Santos, DO1, John G. Quiles, MD2, Jerome C. Edelson, MD3. P2806 - Partial Endoscopic Sleeve Gastroplasty for Management of Gastric Perforation During Intragastric Balloon Placement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Ryan L. Santos, DO1, John G. Quiles, MD2, Jerome C. Edelson, MD3
1San Antonio Uniformed Services Health Education Consortium, San Antonio, TX; 2Brooke Army Medical Center, San Antonio, TX; 3Brooke Army Medical Center, Fort Sam Houston, TX
Introduction: Placement of intragastric balloons (IGB) for weight loss, while generally safe and well tolerated, can lead to rare complications such as gastric perforation. If recognized at the time of placement, the perforation can be managed endoscopically. Here, we present a case of a gastric perforation during IGB placement and its management through endoscopic suturing with conversion to partial Endoscopic Sleeve Gastroplasty (ESG).
Case Description/Methods: A 63-year-old female with a BMI of 35 underwent IGB placement following unsuccessful attempts with lifestyle modifications, phentermine and orlistat. During endoscopy, the IGB was advanced into the stomach and sequentially inflated with 600ml of saline. Immediately following inflation, retroflexion in the body demonstrated a mucosal rent behind the balloon prompting intubation prior to IGB removal (Image A, arrow; Image B). Upon reentering the stomach, a 3 cm full-thickness perforation was identified along the anterior wall. IV antibiotics were given and a surgeon was consulted intraoperatively with plans made for surgery if endoscopic closure was not successful. A dual-channel therapeutic endoscope with suturing device was then introduced and 2 sutures were placed in a running fashion to close the defect (Image C, arrows). Contrast injection into the gastric lumen revealed a residual leak and an additional suture was added for reinforcement in a running fashion akin to ESG. Repeat injection showed no leak. She was admitted for observation.
The following day, she underwent an upper GI series which did not show any extravasation (Image D). Her diet was advanced and she was transitioned to a bariatric diet for six weeks. At two months, she had lost 18 lbs. without further complications.
Discussion: IGB placement is a safe, well-established, and well-tolerated weight loss procedure, but it carries risks inherent to endoscopic interventions. Despite thorough patient selection, including negative Helicobacter pylori status and absence of structural abnormalities or prior gastric/bariatric surgeries, IGB placement resulted in gastric perforation. Prompt recognition, antibiotic administration, surgical consultation, and closure using an endoscopic suture device in a running fashion, akin to ESG, led to favorable outcomes including continued weight loss.
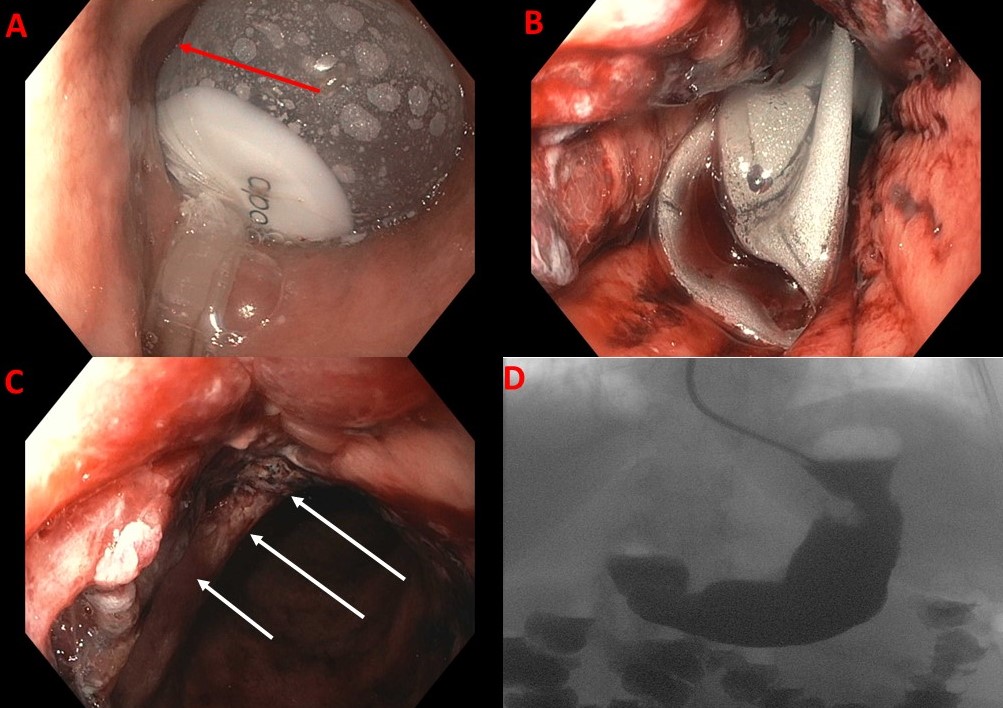
Figure: A: Mucosal rent (arrow) ; B: Prompt IGB removal, C: Defect closure with endoscopic sutures; D: Upper GI series with no evidence of contrast extravasation
Disclosures:
Ryan Santos indicated no relevant financial relationships.
John Quiles indicated no relevant financial relationships.
Jerome Edelson indicated no relevant financial relationships.
Ryan L. Santos, DO1, John G. Quiles, MD2, Jerome C. Edelson, MD3. P2806 - Partial Endoscopic Sleeve Gastroplasty for Management of Gastric Perforation During Intragastric Balloon Placement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

