Monday Poster Session
Category: Interventional Endoscopy
P2807 - An Unusual Case of Metastatic Urothelial Carcinoma With GOO Managed With EUS-GJ
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Zoilo K. Suarez, MD
Florida Atlantic University, Charles E. Schmidt College of Medicine
Boca Raton, FL
Presenting Author(s)
Zoilo K. Suarez, MD1, Celine Vartany, BS1, Finke Ana, MD2, Talwinder Nagi, MD1, Najib Shalabi, MD3, David Forcione, MD4
1Florida Atlantic University, Charles E. Schmidt College of Medicine, Boca Raton, FL; 2Norwalk Hospital, Norwalk, CT; 3Universidad Iberoamericana, Pasadena, CA; 4Boca Raton Regional Hospital, Boca Raton, FL
Introduction: Gastric outlet obstruction (GOO) is a complication of abdominal malignancies in which luminal narrowing results in gastrointestinal symptoms, affecting quality of life. Palliative interventions include surgical gastrojejunostomy (S-GJ) or enteral stent placement (ES). In recent years, endoscopic ultrasound-guided gastrojejunostomy (EUS-GJ) has gained popularity due to lower cost, minimal invasiveness, and durability. We present a patient with metastatic urothelial carcinoma (UC) resulting in GOO who underwent successful EUS-GJ with LAMS placement followed by EUS-guided biliary access.
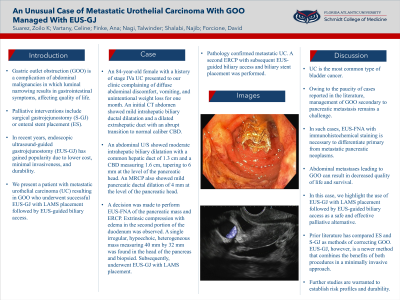
Case Description/Methods: An 84-year-old female with a history of stage IVa UC presented to our clinic complaining of diffuse abdominal discomfort, vomiting, and unintentional weight loss for one month. An initial CT abdomen showed mild intrahepatic biliary ductal dilatation and a dilated extrahepatic duct with an abrupt transition to normal caliber CBD. An abdominal U/S showed moderate intrahepatic biliary dilatation with a common hepatic duct of 1.3 cm and a CBD measuring 1.6 cm, tapering to 6 mm at the level of the pancreatic head. An MRCP also showed mild pancreatic ductal dilation of 4 mm at the level of the pancreatic head. A decision was made to perform EUS-FNA of the pancreatic mass and ERCP. Extrinsic compression with edema in the second portion of the duodenum was observed. A single irregular, hypoechoic, heterogeneous mass measuring 40 mm by 32 mm was found in the head of the pancreas and biopsied. Subsequently, underwent EUS-GJ with LAMS placement. Pathology confirmed metastatic UC. A second ERCP with subsequent EUS-guided biliary access and biliary stent placement was performed.
Discussion: UC is the most common type of bladder cancer. Owing to the paucity of cases reported in the literature, management of GOO secondary to pancreatic metastasis remains a challenge. In such cases, EUS-FNA with immunohistochemical staining is necessary to differentiate primary from metastatic pancreatic neoplasms. Abdominal metastases leading to GOO can result in decreased quality of life and survival. In this case, we highlight the use of EUS-GJ with LAMS placement followed by EUS-guided biliary access as a safe and effective palliative alternative. Prior literature has compared ES and S-GJ as methods of correcting GOO. EUS-GJ, however, is a newer method that combines the benefits of both procedures in a minimally invasive approach. Further studies are warranted to establish risk profiles and durability.

Disclosures:
Zoilo K. Suarez, MD1, Celine Vartany, BS1, Finke Ana, MD2, Talwinder Nagi, MD1, Najib Shalabi, MD3, David Forcione, MD4. P2807 - An Unusual Case of Metastatic Urothelial Carcinoma With GOO Managed With EUS-GJ, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Florida Atlantic University, Charles E. Schmidt College of Medicine, Boca Raton, FL; 2Norwalk Hospital, Norwalk, CT; 3Universidad Iberoamericana, Pasadena, CA; 4Boca Raton Regional Hospital, Boca Raton, FL
Introduction: Gastric outlet obstruction (GOO) is a complication of abdominal malignancies in which luminal narrowing results in gastrointestinal symptoms, affecting quality of life. Palliative interventions include surgical gastrojejunostomy (S-GJ) or enteral stent placement (ES). In recent years, endoscopic ultrasound-guided gastrojejunostomy (EUS-GJ) has gained popularity due to lower cost, minimal invasiveness, and durability. We present a patient with metastatic urothelial carcinoma (UC) resulting in GOO who underwent successful EUS-GJ with LAMS placement followed by EUS-guided biliary access.
Case Description/Methods: An 84-year-old female with a history of stage IVa UC presented to our clinic complaining of diffuse abdominal discomfort, vomiting, and unintentional weight loss for one month. An initial CT abdomen showed mild intrahepatic biliary ductal dilatation and a dilated extrahepatic duct with an abrupt transition to normal caliber CBD. An abdominal U/S showed moderate intrahepatic biliary dilatation with a common hepatic duct of 1.3 cm and a CBD measuring 1.6 cm, tapering to 6 mm at the level of the pancreatic head. An MRCP also showed mild pancreatic ductal dilation of 4 mm at the level of the pancreatic head. A decision was made to perform EUS-FNA of the pancreatic mass and ERCP. Extrinsic compression with edema in the second portion of the duodenum was observed. A single irregular, hypoechoic, heterogeneous mass measuring 40 mm by 32 mm was found in the head of the pancreas and biopsied. Subsequently, underwent EUS-GJ with LAMS placement. Pathology confirmed metastatic UC. A second ERCP with subsequent EUS-guided biliary access and biliary stent placement was performed.
Discussion: UC is the most common type of bladder cancer. Owing to the paucity of cases reported in the literature, management of GOO secondary to pancreatic metastasis remains a challenge. In such cases, EUS-FNA with immunohistochemical staining is necessary to differentiate primary from metastatic pancreatic neoplasms. Abdominal metastases leading to GOO can result in decreased quality of life and survival. In this case, we highlight the use of EUS-GJ with LAMS placement followed by EUS-guided biliary access as a safe and effective palliative alternative. Prior literature has compared ES and S-GJ as methods of correcting GOO. EUS-GJ, however, is a newer method that combines the benefits of both procedures in a minimally invasive approach. Further studies are warranted to establish risk profiles and durability.

Figure: LAMS
Disclosures:
Zoilo Suarez indicated no relevant financial relationships.
Celine Vartany indicated no relevant financial relationships.
Finke Ana indicated no relevant financial relationships.
Talwinder Nagi indicated no relevant financial relationships.
Najib Shalabi indicated no relevant financial relationships.
David Forcione indicated no relevant financial relationships.
Zoilo K. Suarez, MD1, Celine Vartany, BS1, Finke Ana, MD2, Talwinder Nagi, MD1, Najib Shalabi, MD3, David Forcione, MD4. P2807 - An Unusual Case of Metastatic Urothelial Carcinoma With GOO Managed With EUS-GJ, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
