Monday Poster Session
Category: IBD
P2715 - Smoke and Mirrors: Infliximab Biosimilar Induced Pustular Psoriasis After Immunization
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Vini Patel, DO
Atlanta VA Medical Center
Atlanta, GA
Presenting Author(s)
Vini Patel, DO1, Cindy Ye, MD2, Brian Pollack, MD2
1Atlanta VA Medical Center, Atlanta, GA; 2Emory University School of Medicine, Atlanta, GA
Introduction: Non-live vaccines for pneumococcal and herpes zoster are essential for patients with inflammatory bowel disease (IBD). However, the immunocompromised state of patients with IBD on immunosuppression may cause rare reactions. In our case, a patient initially thought to have developed a vaccine-induced rash from shingles vaccine was later diagnosed with infliximab -induced pustular psoriasis following dual vaccination.
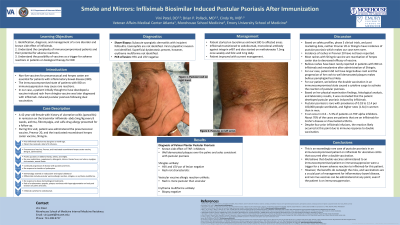
Case Description/Methods: A 42-year-old female with history of ulcerative colitis in remission on infliximab presented for a follow up. At this visit, patient was administered the pneumococcal vaccine and the inactivated recombinant herpes zoster vaccine.The day after, patient developed pruritic pustules on extremities. Patient denied any fevers, oral ulcers, new medications, supplements, or changes in products. Up to this point, she had received four infliximab infusions, with the most recent one a month ago. Patient was empirically started on valacyclovir 1g three times daily for 10 days and clobetasol 0.05% ointment twice daily. Despite completing treatment, rash progressed to well demarcated erythematous plaques, pustules, and hyperpigmented macules. Shave biopsy results were consistent with subacute spongiotic dermatitis and incipient folliculitis. Swabs from the lesions tested negative for herpes simplex virus and varicella-zoster virus via polymerase chain reaction. It was concluded that the patient developed pustular psoriasis induced by infliximab. The immunizations she received may have triggered her hypersensitive immune system causing pustular psoriasis. The patient was initiated on cyclosporine and management of ulcerative colitis was transitioned to vedolizumab.
Discussion: Pustular psoriasis is rare with prevalence of 0.18 to 12.4 per 100,000 people worldwide, and higher rates in women than in men. It can occur in 0.6 – 5.3% of patients on TNF alpha inhibitors. About 70% of the cases are patients that are on infliximab for Crohn’s disease or rheumatoid arthritis. Incidence of rashes in the pneumococcal vaccine have not been reported, and shingles vaccine has rare cases of bullous pemphigoid in immunosuppressed patients but no cases of pustular psoriasis. Case reports of Covid vaccine associated pustular psoriasis have been documented and thought to be due to a cytokine surge, which most likely is the case for our patient after receiving double vaccination while on infliximab. This case represents an exceedingly rare occurrence in an immunocompromised patient.
Disclosures:
Vini Patel, DO1, Cindy Ye, MD2, Brian Pollack, MD2. P2715 - Smoke and Mirrors: Infliximab Biosimilar Induced Pustular Psoriasis After Immunization, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Atlanta VA Medical Center, Atlanta, GA; 2Emory University School of Medicine, Atlanta, GA
Introduction: Non-live vaccines for pneumococcal and herpes zoster are essential for patients with inflammatory bowel disease (IBD). However, the immunocompromised state of patients with IBD on immunosuppression may cause rare reactions. In our case, a patient initially thought to have developed a vaccine-induced rash from shingles vaccine was later diagnosed with infliximab -induced pustular psoriasis following dual vaccination.
Case Description/Methods: A 42-year-old female with history of ulcerative colitis in remission on infliximab presented for a follow up. At this visit, patient was administered the pneumococcal vaccine and the inactivated recombinant herpes zoster vaccine.The day after, patient developed pruritic pustules on extremities. Patient denied any fevers, oral ulcers, new medications, supplements, or changes in products. Up to this point, she had received four infliximab infusions, with the most recent one a month ago. Patient was empirically started on valacyclovir 1g three times daily for 10 days and clobetasol 0.05% ointment twice daily. Despite completing treatment, rash progressed to well demarcated erythematous plaques, pustules, and hyperpigmented macules. Shave biopsy results were consistent with subacute spongiotic dermatitis and incipient folliculitis. Swabs from the lesions tested negative for herpes simplex virus and varicella-zoster virus via polymerase chain reaction. It was concluded that the patient developed pustular psoriasis induced by infliximab. The immunizations she received may have triggered her hypersensitive immune system causing pustular psoriasis. The patient was initiated on cyclosporine and management of ulcerative colitis was transitioned to vedolizumab.
Discussion: Pustular psoriasis is rare with prevalence of 0.18 to 12.4 per 100,000 people worldwide, and higher rates in women than in men. It can occur in 0.6 – 5.3% of patients on TNF alpha inhibitors. About 70% of the cases are patients that are on infliximab for Crohn’s disease or rheumatoid arthritis. Incidence of rashes in the pneumococcal vaccine have not been reported, and shingles vaccine has rare cases of bullous pemphigoid in immunosuppressed patients but no cases of pustular psoriasis. Case reports of Covid vaccine associated pustular psoriasis have been documented and thought to be due to a cytokine surge, which most likely is the case for our patient after receiving double vaccination while on infliximab. This case represents an exceedingly rare occurrence in an immunocompromised patient.
Disclosures:
Vini Patel indicated no relevant financial relationships.
Cindy Ye indicated no relevant financial relationships.
Brian Pollack indicated no relevant financial relationships.
Vini Patel, DO1, Cindy Ye, MD2, Brian Pollack, MD2. P2715 - Smoke and Mirrors: Infliximab Biosimilar Induced Pustular Psoriasis After Immunization, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

