Monday Poster Session
Category: IBD
P2719 - Paradoxical Psoriasis and Alopecia Areata After the Use of Anti-TNF in a Patient With Crohn's Cisease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ahmad Alomari, MD
Henry Ford Hospital
Detroit, MI
Presenting Author(s)
Ahmad Alomari, MD1, Mohammed Abusuliman, MD2, Abdulmalik Saleem, MD2, Allison N. Malick, MD2, Diana Jomaa, MD2, Ismail Althunibat, MD3, Iana Gueorguieva, MD4
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Health, Detroit, MI; 3Saint Michael's Medical Center, Newark, NJ; 4Henry Ford Health, Novi, MI
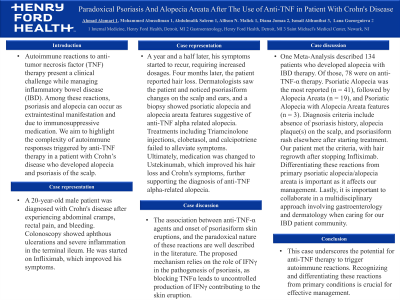
Introduction: Autoimmune reactions to anti-tumor necrosis factor (TNF) therapy present a clinical challenge while managing inflammatory bowel disease (IBD). Among these reactions, psoriasis and alopecia can occur as extraintestinal manifestation and due to immunosuppressive medication. We aim to highlight the complexity of autoimmune responses triggered by anti-TNF therapy in a patient with Crohn’s disease who developed alopecia and psoriasis of the scalp.
Case Description/Methods: A 20-year-old male patient was diagnosed with Crohn's disease after experiencing abdominal cramps, rectal pain, and bleeding. Colonoscopy showed aphthous ulcerations and severe inflammation in the terminal ileum. He was started on Infliximab, which improved his symptoms. A year and a half later, his symptoms started to recur, requiring increased dosages. Four months later, the patient reported hair loss. Dermatologists saw the patient and noticed psoriasiform changes on the scalp and ears, and a biopsy showed psoriatic alopecia and alopecia areata features suggestive of anti-TNF alpha related alopecia. Treatments including Triamcinolone injections, clobetasol, and calcipotriene failed to alleviate symptoms. Ultimately, medication was changed to Ustekinumab, which improved his hair loss and Crohn's symptoms, further supporting the diagnosis of anti-TNF alpha-related alopecia.
Discussion: The association between anti-TNF-α agents and onset of psoriasiform skin eruptions, and the paradoxical nature of these reactions are well described in the literature. The proposed mechanism relies on the role of IFNγ in the pathogenesis of psoriasis, as blocking TNFα leads to uncontrolled production of IFNγ contributing to the skin eruption. One Meta-Analysis described 134 patients who developed alopecia with IBD therapy. Of those, 78 were on anti-TNF-α therapy. Psoriatic Alopecia was the most reported (n = 41), followed by Alopecia Areata (n = 19), and Psoriatic Alopecia with Alopecia Areata features (n = 3). Diagnosis criteria include absence of psoriasis history, alopecia plaque(s) on the scalp, and psoriasiform rash elsewhere after starting treatment. Our patient met the criteria, with hair regrowth after stopping Infliximab. Differentiating these reactions from primary psoriatic alopecia/alopecia areata is important as it affects our management. Lastly, it is important to collaborate in a multidisciplinary approach involving gastroenterology and dermatology when caring for our IBD patient community.
Disclosures:
Ahmad Alomari, MD1, Mohammed Abusuliman, MD2, Abdulmalik Saleem, MD2, Allison N. Malick, MD2, Diana Jomaa, MD2, Ismail Althunibat, MD3, Iana Gueorguieva, MD4. P2719 - Paradoxical Psoriasis and Alopecia Areata After the Use of Anti-TNF in a Patient With Crohn's Cisease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Health, Detroit, MI; 3Saint Michael's Medical Center, Newark, NJ; 4Henry Ford Health, Novi, MI
Introduction: Autoimmune reactions to anti-tumor necrosis factor (TNF) therapy present a clinical challenge while managing inflammatory bowel disease (IBD). Among these reactions, psoriasis and alopecia can occur as extraintestinal manifestation and due to immunosuppressive medication. We aim to highlight the complexity of autoimmune responses triggered by anti-TNF therapy in a patient with Crohn’s disease who developed alopecia and psoriasis of the scalp.
Case Description/Methods: A 20-year-old male patient was diagnosed with Crohn's disease after experiencing abdominal cramps, rectal pain, and bleeding. Colonoscopy showed aphthous ulcerations and severe inflammation in the terminal ileum. He was started on Infliximab, which improved his symptoms. A year and a half later, his symptoms started to recur, requiring increased dosages. Four months later, the patient reported hair loss. Dermatologists saw the patient and noticed psoriasiform changes on the scalp and ears, and a biopsy showed psoriatic alopecia and alopecia areata features suggestive of anti-TNF alpha related alopecia. Treatments including Triamcinolone injections, clobetasol, and calcipotriene failed to alleviate symptoms. Ultimately, medication was changed to Ustekinumab, which improved his hair loss and Crohn's symptoms, further supporting the diagnosis of anti-TNF alpha-related alopecia.
Discussion: The association between anti-TNF-α agents and onset of psoriasiform skin eruptions, and the paradoxical nature of these reactions are well described in the literature. The proposed mechanism relies on the role of IFNγ in the pathogenesis of psoriasis, as blocking TNFα leads to uncontrolled production of IFNγ contributing to the skin eruption. One Meta-Analysis described 134 patients who developed alopecia with IBD therapy. Of those, 78 were on anti-TNF-α therapy. Psoriatic Alopecia was the most reported (n = 41), followed by Alopecia Areata (n = 19), and Psoriatic Alopecia with Alopecia Areata features (n = 3). Diagnosis criteria include absence of psoriasis history, alopecia plaque(s) on the scalp, and psoriasiform rash elsewhere after starting treatment. Our patient met the criteria, with hair regrowth after stopping Infliximab. Differentiating these reactions from primary psoriatic alopecia/alopecia areata is important as it affects our management. Lastly, it is important to collaborate in a multidisciplinary approach involving gastroenterology and dermatology when caring for our IBD patient community.
Disclosures:
Ahmad Alomari indicated no relevant financial relationships.
Mohammed Abusuliman indicated no relevant financial relationships.
Abdulmalik Saleem indicated no relevant financial relationships.
Allison Malick indicated no relevant financial relationships.
Diana Jomaa indicated no relevant financial relationships.
Ismail Althunibat indicated no relevant financial relationships.
Iana Gueorguieva indicated no relevant financial relationships.
Ahmad Alomari, MD1, Mohammed Abusuliman, MD2, Abdulmalik Saleem, MD2, Allison N. Malick, MD2, Diana Jomaa, MD2, Ismail Althunibat, MD3, Iana Gueorguieva, MD4. P2719 - Paradoxical Psoriasis and Alopecia Areata After the Use of Anti-TNF in a Patient With Crohn's Cisease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
