Monday Poster Session
Category: IBD
P2720 - Complicated Case of Diverticulitis Turned Crohn’s
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Regis Lee, DO
HCA Riverside Community Hospital
Riverside, CA
Presenting Author(s)
Regis Lee, DO, Alex Prevallet, DO, Carol Monis, MD, Anas Kawayeh, MD
HCA Riverside Community Hospital, Riverside, CA
Introduction: Inflammatory bowel disease (IBD) can often masquerade as diverticulitis. This report represents a complicated case of recurrent diverticulitis that led to newly discovered Crohn’s disease.
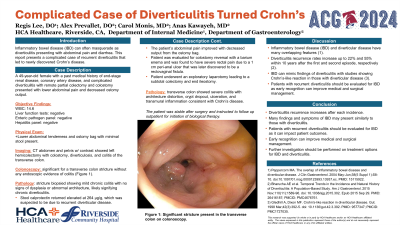
Case Description/Methods: A 49-year-old female with a past medical history of end-stage renal disease, coronary artery disease, and complicated diverticulitis with remote partial colectomy and colostomy presented with lower abdominal pain and decreased ostomy output. She had a recent discharge after being treated for a presumed episode of diverticulitis. She denied family history of IBD and personal history of Clostridium difficile (C. diff). Her last colonoscopy was prior to her colectomy and was normal, except for diverticulosis. On presentation, she had a leukocytosis of 14.6. Her liver enzymes, stool enteric pathogen panel, and hepatitis panel were unrevealing. Physical exam was pertinent for lower abdominal tenderness and a left lower quadrant ostomy bag with stool present. CT abdomen showed left hemicolectomy with colostomy, diverticulosis, and colitis of the transverse colon. Colonoscopy was significant for a large transverse colon stricture without any endoscopic evidence of colitis. Pathology from the stricture was obtained, showing mild chronic colitis with no signs of dysplasia or abnormal architecture, likely signifying chronic diverticulitis. Stool calprotectin returned elevated at 264, which was suspected to be due to recurrent diverticular disease. The patient’s abdominal pain improved with decreased output from the ostomy bag. The patient was evaluated for colostomy reversal with a barium enema, and was found to have severe rectal pain due to a 1 cm peri-anal ulcer that was later discovered to be a rectovaginal fistula. The patient then underwent an exploratory laparotomy leading to a subtotal colectomy and end ileostomy. Pathology of the transverse colon showed severe colitis with architecture distortion, crypt dropout, ulceration, and transmural inflammation consistent with Crohn’s disease. The patient was stable after surgery and instructed to follow up outpatient for initiation of biological therapy.
Discussion: Diverticulitis recurrence rates increase up to 22% and 55% within 10 years after the first and second episode, respectively. IBD can mimic findings of diverticulitis with studies showing Crohn’s-like reaction in those with diverticular disease. Patients with recurrent diverticulitis should be evaluated for IBD as early recognition can affect medical and surgical management.

Disclosures:
Regis Lee, DO, Alex Prevallet, DO, Carol Monis, MD, Anas Kawayeh, MD. P2720 - Complicated Case of Diverticulitis Turned Crohn’s, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
HCA Riverside Community Hospital, Riverside, CA
Introduction: Inflammatory bowel disease (IBD) can often masquerade as diverticulitis. This report represents a complicated case of recurrent diverticulitis that led to newly discovered Crohn’s disease.
Case Description/Methods: A 49-year-old female with a past medical history of end-stage renal disease, coronary artery disease, and complicated diverticulitis with remote partial colectomy and colostomy presented with lower abdominal pain and decreased ostomy output. She had a recent discharge after being treated for a presumed episode of diverticulitis. She denied family history of IBD and personal history of Clostridium difficile (C. diff). Her last colonoscopy was prior to her colectomy and was normal, except for diverticulosis. On presentation, she had a leukocytosis of 14.6. Her liver enzymes, stool enteric pathogen panel, and hepatitis panel were unrevealing. Physical exam was pertinent for lower abdominal tenderness and a left lower quadrant ostomy bag with stool present. CT abdomen showed left hemicolectomy with colostomy, diverticulosis, and colitis of the transverse colon. Colonoscopy was significant for a large transverse colon stricture without any endoscopic evidence of colitis. Pathology from the stricture was obtained, showing mild chronic colitis with no signs of dysplasia or abnormal architecture, likely signifying chronic diverticulitis. Stool calprotectin returned elevated at 264, which was suspected to be due to recurrent diverticular disease. The patient’s abdominal pain improved with decreased output from the ostomy bag. The patient was evaluated for colostomy reversal with a barium enema, and was found to have severe rectal pain due to a 1 cm peri-anal ulcer that was later discovered to be a rectovaginal fistula. The patient then underwent an exploratory laparotomy leading to a subtotal colectomy and end ileostomy. Pathology of the transverse colon showed severe colitis with architecture distortion, crypt dropout, ulceration, and transmural inflammation consistent with Crohn’s disease. The patient was stable after surgery and instructed to follow up outpatient for initiation of biological therapy.
Discussion: Diverticulitis recurrence rates increase up to 22% and 55% within 10 years after the first and second episode, respectively. IBD can mimic findings of diverticulitis with studies showing Crohn’s-like reaction in those with diverticular disease. Patients with recurrent diverticulitis should be evaluated for IBD as early recognition can affect medical and surgical management.

Figure: Large stricture present in the transverse colon on colonoscopy.
Disclosures:
Regis Lee indicated no relevant financial relationships.
Alex Prevallet indicated no relevant financial relationships.
Carol Monis indicated no relevant financial relationships.
Anas Kawayeh indicated no relevant financial relationships.
Regis Lee, DO, Alex Prevallet, DO, Carol Monis, MD, Anas Kawayeh, MD. P2720 - Complicated Case of Diverticulitis Turned Crohn’s, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
