Monday Poster Session
Category: IBD
P2722 - Immune Checkpoint Inhibitors Leading to Refractory Primary UC Flare Requiring Diverting Ileostomy With Long-Term Adjuvant Biological Therapy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Divya Roy, DO
NYU Langone Health
Mineola, NY
Presenting Author(s)
Divya Roy, DO1, Aniza Nasir, BS, MS2, Bradley Morganstern, MD1, Zinal Patel, MD1, Patrick Hartendorp, MD1, Zarrin Hossein-Zadeh, MD1
1NYU Langone Health, Mineola, NY; 2Rutgers Biomedical and Health Sciences, Newark, NJ
Introduction: A well-studied adverse effect of immune checkpoint inhibitors (ICI) is checkpoint-induced colitis (CIC), a characteristic immune-related adverse effect (irAEs), and is phenotypically indistinguishable from ulcerative colitis (UC) flares. First-line therapy for both conditions is corticosteroid but can escalate to immunotherapy, i.e. infliximab, if refractory. Management becomes complicated when patients have contraindications to infliximab. We present the case of a 28-year-old male with UC who was started on ipilimumab for metastatic melanoma and developed refractory primary ulcerative colitis flare.
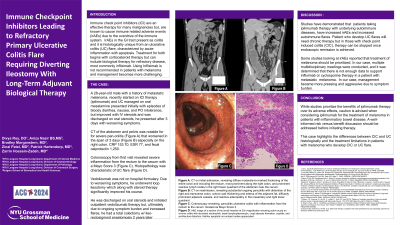
Case Description/Methods: A 28-year-old male with a history of UC on PO mesalamine, and metastatic melanoma presented with episodes of bloody diarrhea, nausea, malaise, and PO intolerance. He was recently started on ICI therapy, ipilimumab, for metastatic melanoma. CT of the abdomen and pelvis was notable for acute interstitial pancreatitis and severe pan-colitis (Figure A). Labs were remarkable for CRP 153.70, ESR 77, and fecal calprotectin 1,250.
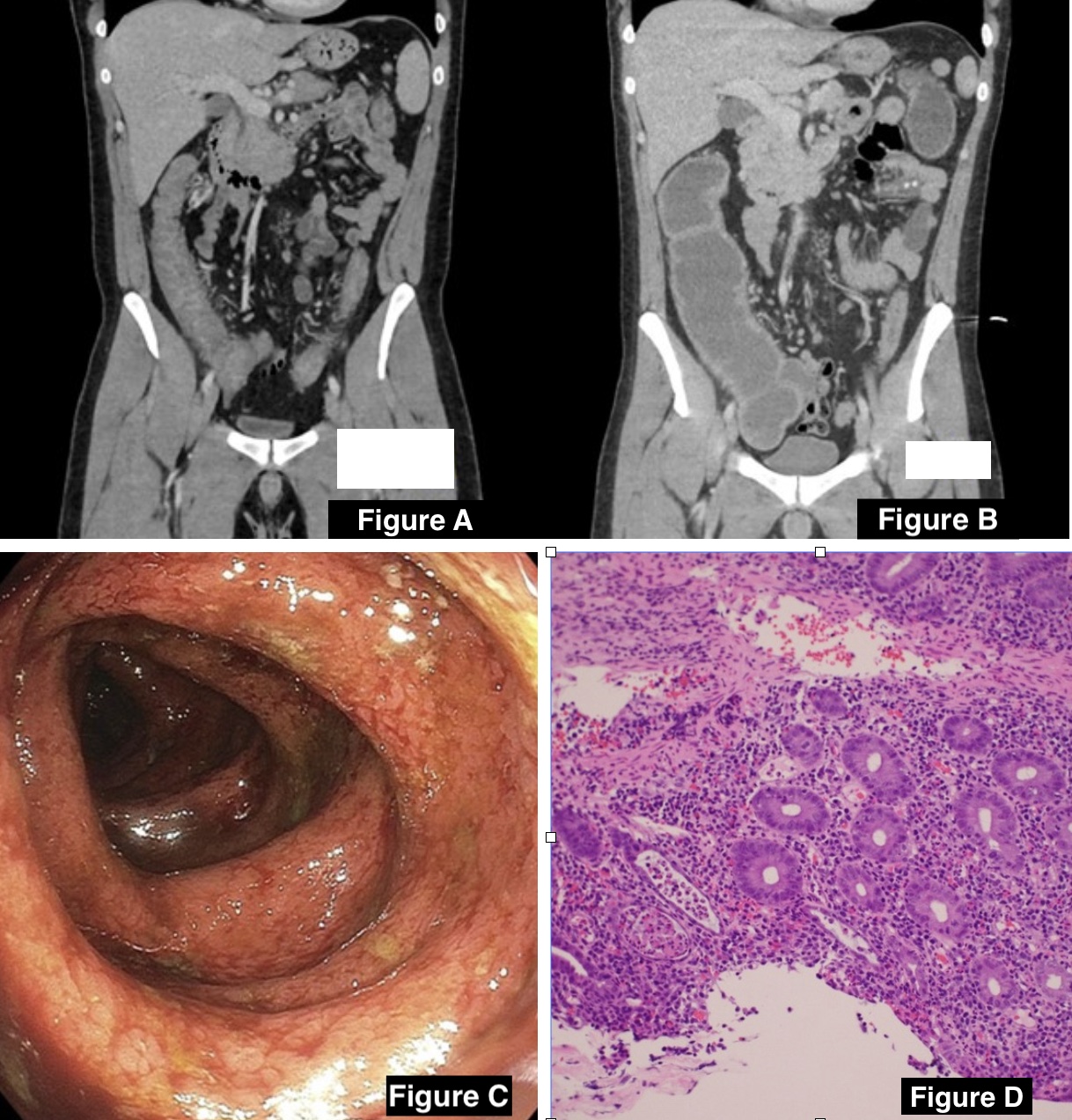
Colonoscopy revealed severe inflammation from the rectum to the cecum (Mayo Score 3) (Figure C). Segmental biopsies were characteristic of UC flare (Figure D). The patient was started on IV steroids and discharged home on an oral taper. The patient returned 3 days later with worsening abdominal pain, bloody bowel movements, and CT findings (Figure B). Steroid therapy was attempted with no improvement in symptoms. Infliximab and cyclosporine therapy was not advised due to history of metastatic melanoma. After a multidisciplinary meeting, the patient underwent a loop ileostomy and transitioned from IV to oral steroids post-op day two. He was discharged with a steroid taper with planned Vedolizumab initiation and ostomy takedown as an outpatient. Three months after discharge from the hospital, his IBD symptoms remained controlled, and he was continued on vedolizumab.
Discussion: There is limited data on the risk of irAEs in patients with a history of IBD, however, the incidence of irAEs is generally higher in these patients. Though both conditions present similarly, the histopathologic differences are used to diagnose the underlying disease.
This case highlights the treatment limitation in patients with melanoma who develop CIC and UC flare. Caution is advised when considering ipilimumab for the treatment of melanoma in patients with inflammatory bowel disease. A well-informed risk versus benefit discussion should be addressed before initiating therapy.
Disclosures:
Divya Roy, DO1, Aniza Nasir, BS, MS2, Bradley Morganstern, MD1, Zinal Patel, MD1, Patrick Hartendorp, MD1, Zarrin Hossein-Zadeh, MD1. P2722 - Immune Checkpoint Inhibitors Leading to Refractory Primary UC Flare Requiring Diverting Ileostomy With Long-Term Adjuvant Biological Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1NYU Langone Health, Mineola, NY; 2Rutgers Biomedical and Health Sciences, Newark, NJ
Introduction: A well-studied adverse effect of immune checkpoint inhibitors (ICI) is checkpoint-induced colitis (CIC), a characteristic immune-related adverse effect (irAEs), and is phenotypically indistinguishable from ulcerative colitis (UC) flares. First-line therapy for both conditions is corticosteroid but can escalate to immunotherapy, i.e. infliximab, if refractory. Management becomes complicated when patients have contraindications to infliximab. We present the case of a 28-year-old male with UC who was started on ipilimumab for metastatic melanoma and developed refractory primary ulcerative colitis flare.
Case Description/Methods: A 28-year-old male with a history of UC on PO mesalamine, and metastatic melanoma presented with episodes of bloody diarrhea, nausea, malaise, and PO intolerance. He was recently started on ICI therapy, ipilimumab, for metastatic melanoma. CT of the abdomen and pelvis was notable for acute interstitial pancreatitis and severe pan-colitis (Figure A). Labs were remarkable for CRP 153.70, ESR 77, and fecal calprotectin 1,250.
Colonoscopy revealed severe inflammation from the rectum to the cecum (Mayo Score 3) (Figure C). Segmental biopsies were characteristic of UC flare (Figure D). The patient was started on IV steroids and discharged home on an oral taper. The patient returned 3 days later with worsening abdominal pain, bloody bowel movements, and CT findings (Figure B). Steroid therapy was attempted with no improvement in symptoms. Infliximab and cyclosporine therapy was not advised due to history of metastatic melanoma. After a multidisciplinary meeting, the patient underwent a loop ileostomy and transitioned from IV to oral steroids post-op day two. He was discharged with a steroid taper with planned Vedolizumab initiation and ostomy takedown as an outpatient. Three months after discharge from the hospital, his IBD symptoms remained controlled, and he was continued on vedolizumab.
Discussion: There is limited data on the risk of irAEs in patients with a history of IBD, however, the incidence of irAEs is generally higher in these patients. Though both conditions present similarly, the histopathologic differences are used to diagnose the underlying disease.
This case highlights the treatment limitation in patients with melanoma who develop CIC and UC flare. Caution is advised when considering ipilimumab for the treatment of melanoma in patients with inflammatory bowel disease. A well-informed risk versus benefit discussion should be addressed before initiating therapy.
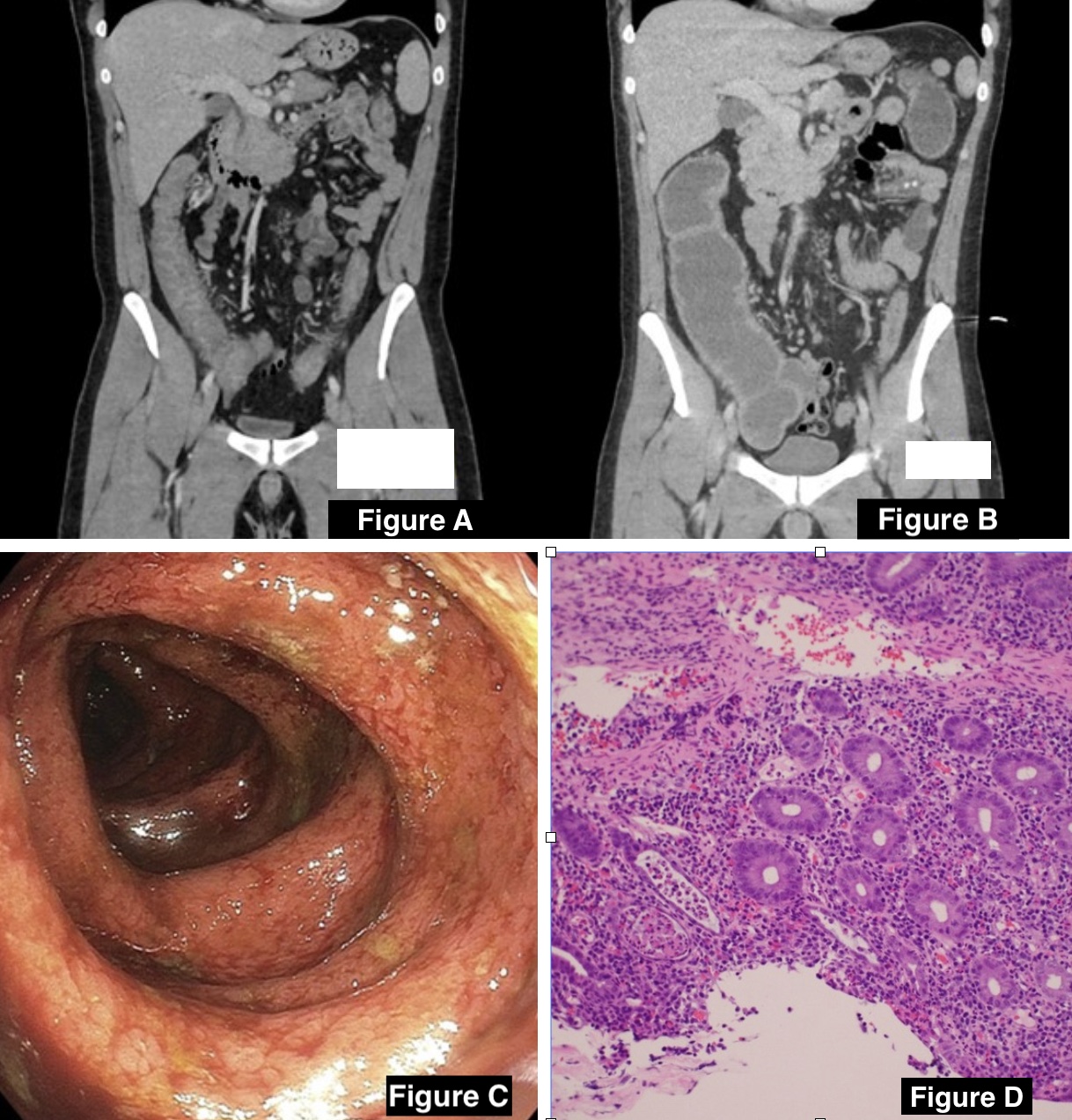
Figure: Figure A: CT on initial admission, revealing diffuse moderate-to-marked thickening of the entire colon and including the rectum, most prominent along the right colon, and prominent reactive lymph nodes in the right lower quadrant of the abdomen near the cecum.
Figure B: CT on readmission, revealing substantial ongoing pancolitis with distention of the right and transverse colon, colonic wall thickening and edema of the adjacent fat, diffusely prominent adjacent vessels, and reactive adenopathy in the mesentery and right lower quadrant.
Figure C: Colonoscopy revealing, Pancolitis ulcerative colitis with inflammation from the rectum to the cecum. Graded as Mayo Score 3
Figure D: H&E image of a section of the small intestine at 20x magnification showing active acute on chronic colitis with abundant neutrophils, basal lymphoplasmacytic, crypt abscess formation, cryptitis, and architecture distortion. Neither apoptotic nor ectopic bodies appreciated
Figure B: CT on readmission, revealing substantial ongoing pancolitis with distention of the right and transverse colon, colonic wall thickening and edema of the adjacent fat, diffusely prominent adjacent vessels, and reactive adenopathy in the mesentery and right lower quadrant.
Figure C: Colonoscopy revealing, Pancolitis ulcerative colitis with inflammation from the rectum to the cecum. Graded as Mayo Score 3
Figure D: H&E image of a section of the small intestine at 20x magnification showing active acute on chronic colitis with abundant neutrophils, basal lymphoplasmacytic, crypt abscess formation, cryptitis, and architecture distortion. Neither apoptotic nor ectopic bodies appreciated
Disclosures:
Divya Roy indicated no relevant financial relationships.
Aniza Nasir indicated no relevant financial relationships.
Bradley Morganstern indicated no relevant financial relationships.
Zinal Patel indicated no relevant financial relationships.
Patrick Hartendorp indicated no relevant financial relationships.
Zarrin Hossein-Zadeh indicated no relevant financial relationships.
Divya Roy, DO1, Aniza Nasir, BS, MS2, Bradley Morganstern, MD1, Zinal Patel, MD1, Patrick Hartendorp, MD1, Zarrin Hossein-Zadeh, MD1. P2722 - Immune Checkpoint Inhibitors Leading to Refractory Primary UC Flare Requiring Diverting Ileostomy With Long-Term Adjuvant Biological Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
