Monday Poster Session
Category: IBD
P2727 - Hemorrhagic Shock as the Initial Presentation of Stricturing Crohn's Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MS
Matt Sumethasorn, MD
Keck School of Medicine of the University of Southern California
Los Angeles, CA
Presenting Author(s)
Matt Sumethasorn, MD, Patrick Lee, MD, Neel K. Mann, MD, MPH, Guang-Qian Xiao, MD, Bing Zhang, MD
Keck School of Medicine of the University of Southern California, Los Angeles, CA
Introduction: Hematochezia is common in Crohn disease, but severe gastrointestinal (GI) hemorrhage causing hemodynamic instability is rare. Stricturing disease often presents with obstruction, not bleeding. This case underscores a rare but severe presentation of stricturing Crohn disease causing hemorrhagic shock and highlights the diagnostic value of small bowel enteroscopy.
Case Description/Methods: A 30-year-old Korean American man with no prior medical history presented with one week of melena, abdominal discomfort, and nausea. Initial hemoglobin was 10.9 g/dL and he was hemodynamically stable. The next day he experienced a syncopal episode with acute hypotension with significant bloody stool output, requiring intensive care for vasopressors where he received 9 units of packed RBCs. CT angiography showed no active bleeding. Endoscopy revealed mild gastritis; colonoscopy showed blood-filled colon up to the distal ileum. A tagged RBC scan ruled out Meckel’s diverticulum.
Magnetic resonance enterography showed no abnormalities, but capsule endoscopy identified multiple ulcerated strictures, with capsule retention. Double balloon enteroscopy confirmed five distal ileal strictures. Due to the initial presentation of hemorrhagic shock, the consensus at our hospital’s multidisciplinary IBD conference was to proceed with laparoscopic small bowel resection. A Pathology confirmed chronic ileitis with no granulomas or dysplasia. Post-operatively, the patient started on infliximab for Crohn disease management.
Discussion: Significant GI bleeding in Crohn disease commonly arises from transmural inflammation and focal erosion into a nearby vessel, though this has rarely ever been described in the context of strictures. A pediatric case series highlighted three patients with intestinal strictures that presented with GI bleeding without signs of obstruction, but the etiologies of these strictures were suspected to be from necrotizing enterocolitis. Furthermore, all three cases presented as chronic GI bleeding and did not cause hemodynamic compromise. To our knowledge, this is the first documented case in the literature of stricturing Crohn disease causing profuse bleeding and hemorrhagic shock. Severe GI bleeding lacks standardized management guidelines, with decisions based on symptoms, severity, and complications risk. Surgical resection was chosen to prevent recurrence and manage future complications, considering high rebleeding rates in non-operative patients.
Disclosures:
Matt Sumethasorn, MD, Patrick Lee, MD, Neel K. Mann, MD, MPH, Guang-Qian Xiao, MD, Bing Zhang, MD. P2727 - Hemorrhagic Shock as the Initial Presentation of Stricturing Crohn's Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Keck School of Medicine of the University of Southern California, Los Angeles, CA
Introduction: Hematochezia is common in Crohn disease, but severe gastrointestinal (GI) hemorrhage causing hemodynamic instability is rare. Stricturing disease often presents with obstruction, not bleeding. This case underscores a rare but severe presentation of stricturing Crohn disease causing hemorrhagic shock and highlights the diagnostic value of small bowel enteroscopy.
Case Description/Methods: A 30-year-old Korean American man with no prior medical history presented with one week of melena, abdominal discomfort, and nausea. Initial hemoglobin was 10.9 g/dL and he was hemodynamically stable. The next day he experienced a syncopal episode with acute hypotension with significant bloody stool output, requiring intensive care for vasopressors where he received 9 units of packed RBCs. CT angiography showed no active bleeding. Endoscopy revealed mild gastritis; colonoscopy showed blood-filled colon up to the distal ileum. A tagged RBC scan ruled out Meckel’s diverticulum.
Magnetic resonance enterography showed no abnormalities, but capsule endoscopy identified multiple ulcerated strictures, with capsule retention. Double balloon enteroscopy confirmed five distal ileal strictures. Due to the initial presentation of hemorrhagic shock, the consensus at our hospital’s multidisciplinary IBD conference was to proceed with laparoscopic small bowel resection. A Pathology confirmed chronic ileitis with no granulomas or dysplasia. Post-operatively, the patient started on infliximab for Crohn disease management.
Discussion: Significant GI bleeding in Crohn disease commonly arises from transmural inflammation and focal erosion into a nearby vessel, though this has rarely ever been described in the context of strictures. A pediatric case series highlighted three patients with intestinal strictures that presented with GI bleeding without signs of obstruction, but the etiologies of these strictures were suspected to be from necrotizing enterocolitis. Furthermore, all three cases presented as chronic GI bleeding and did not cause hemodynamic compromise. To our knowledge, this is the first documented case in the literature of stricturing Crohn disease causing profuse bleeding and hemorrhagic shock. Severe GI bleeding lacks standardized management guidelines, with decisions based on symptoms, severity, and complications risk. Surgical resection was chosen to prevent recurrence and manage future complications, considering high rebleeding rates in non-operative patients.
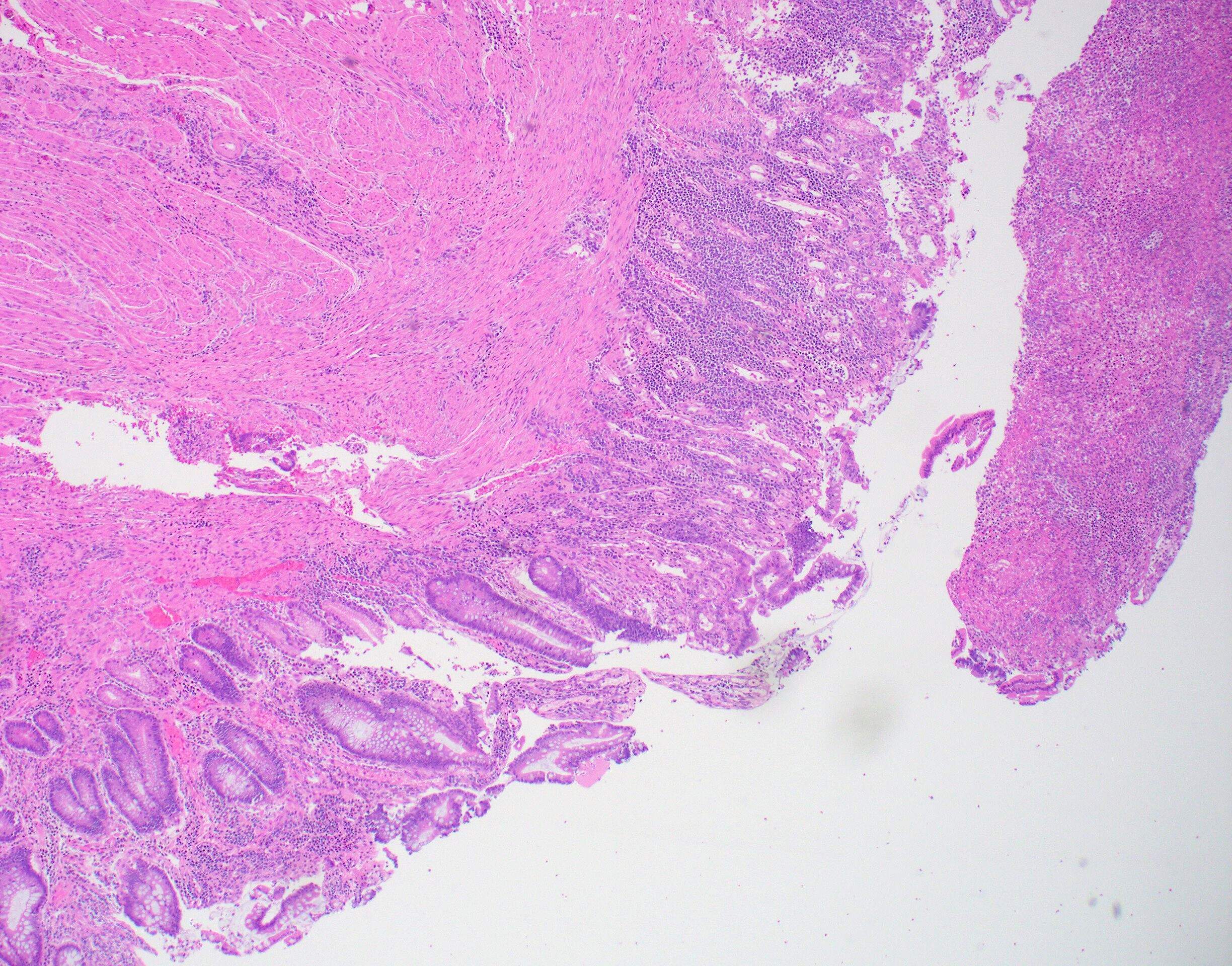
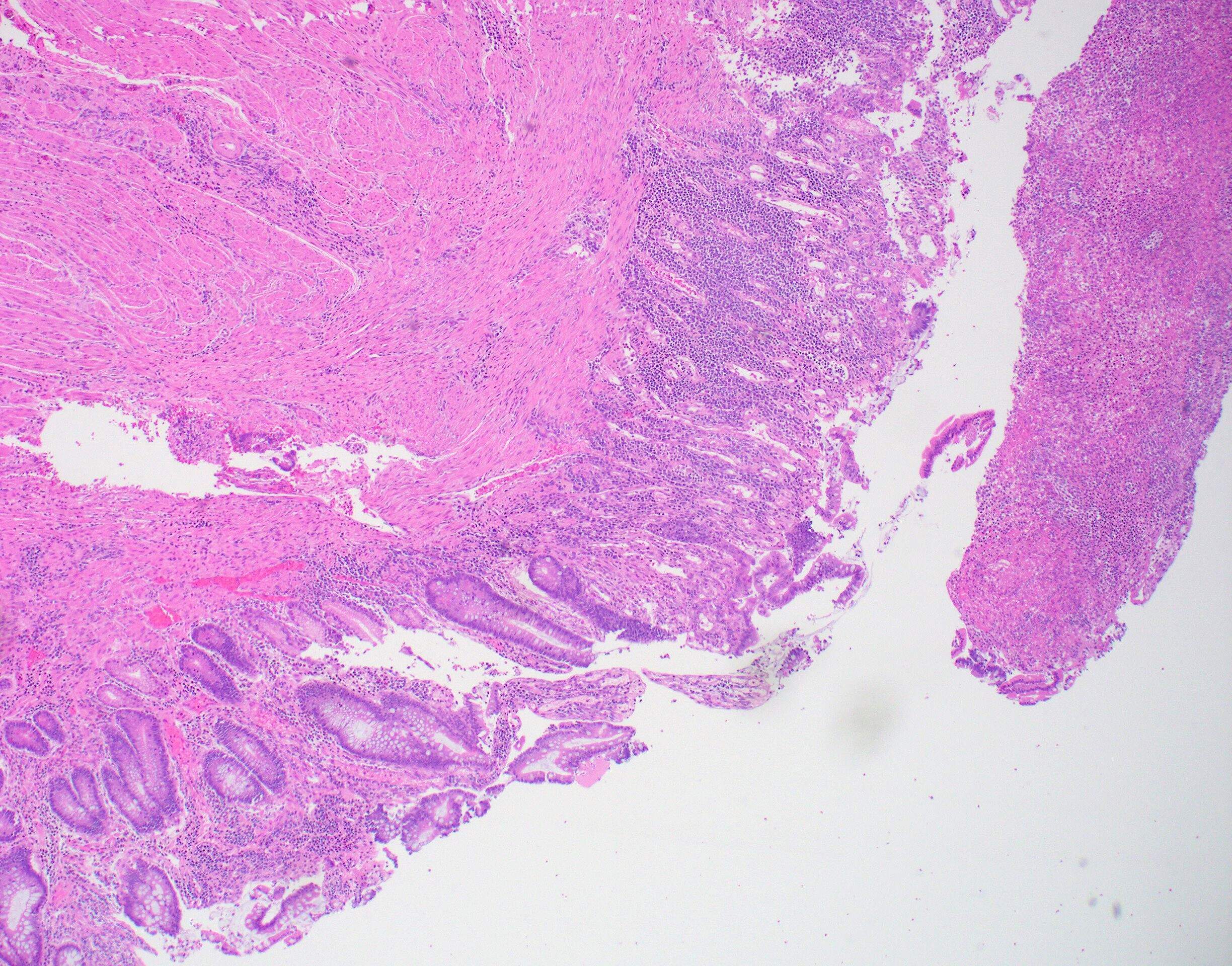
Figure: Figure 1: Crypt drop off and architecture distortion and basal dense lymphoplasmacytic infiltration.
Disclosures:
Matt Sumethasorn indicated no relevant financial relationships.
Patrick Lee indicated no relevant financial relationships.
Neel Mann indicated no relevant financial relationships.
Guang-Qian Xiao indicated no relevant financial relationships.
Bing Zhang indicated no relevant financial relationships.
Matt Sumethasorn, MD, Patrick Lee, MD, Neel K. Mann, MD, MPH, Guang-Qian Xiao, MD, Bing Zhang, MD. P2727 - Hemorrhagic Shock as the Initial Presentation of Stricturing Crohn's Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
