Monday Poster Session
Category: IBD
P2728 - Upadacitinib for Severe Crohn's-Like Enteritis Following Colectomy for Ulcerative Colitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Leona Chan, MD
University of Alberta
Edmonton, AB, Canada
Presenting Author(s)
Leona Chan, MD1, Eric Lam, MD,2, Yvette Leung, MD3, Jeremy Liu Chen Kiow, MD2
1University of Alberta, Edmonton, AB, Canada; 2University of British Columbia, Vancouver, BC, Canada; 3University of British Columbia, IBD Centre of BC, Vancouver, BC, Canada
Introduction: Ulcerative colitis (UC) is an inflammatory condition typically confined to the rectum and colon. Occasionally, the small bowel can be affected with multiple well-described variants including backwash ileitis, post-colectomy pouchitis and enteritis in UC. In recent decades, several case reports have described a distinctive form of fulminant enteritis following colectomy in UC patients, known as postcolectomy enteritis (PCE), requiring corticosteroid induction and immunosuppressive maintenance therapy. However, the pathogenesis of PCE, its association with UC or Crohn’s Disease (CD), and optimal therapy remains unclear.
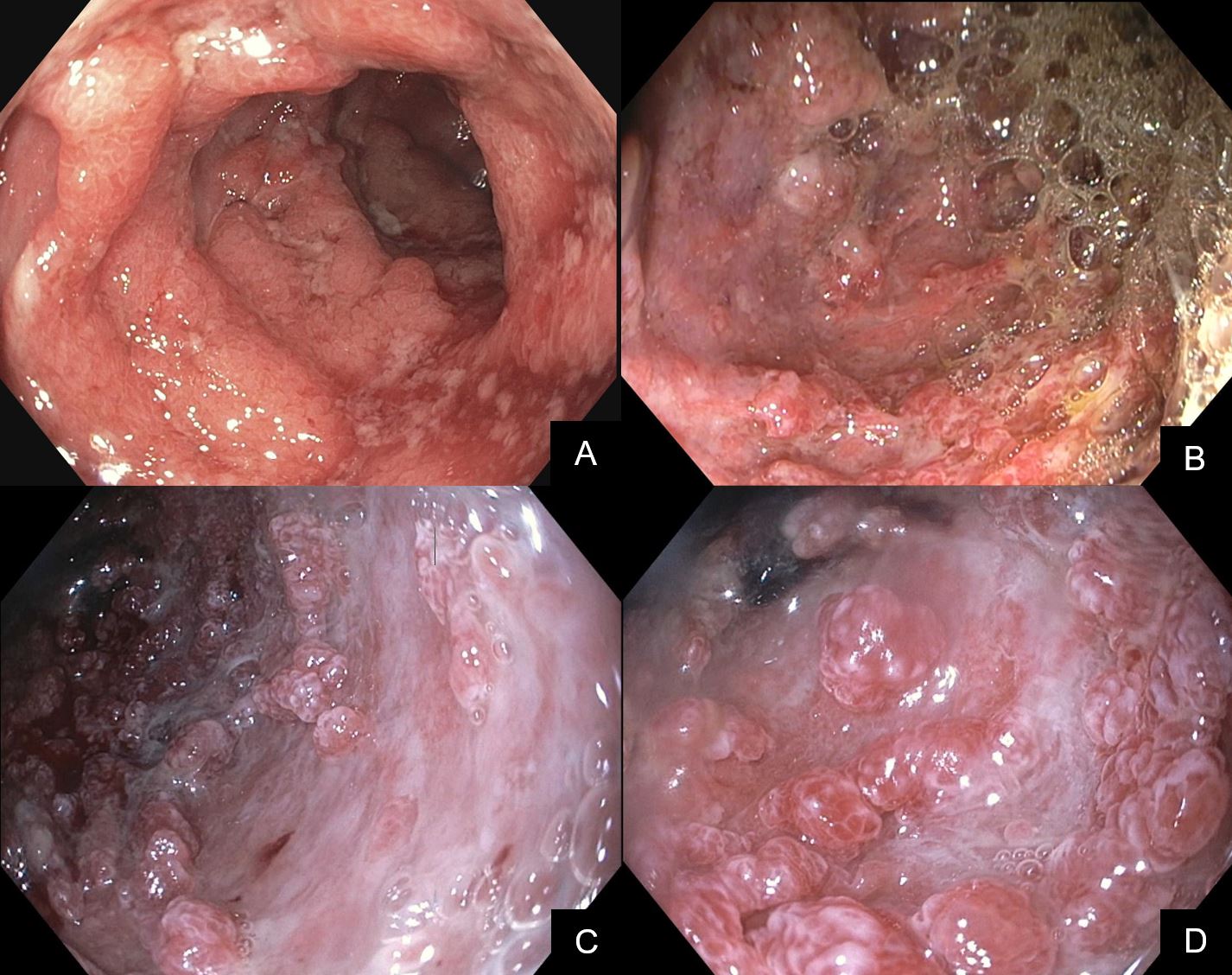
Case Description/Methods: We present a 23-year-old female initially diagnosed with UC in October 2022 based on imaging, endoscopic and pathology findings, who underwent total colectomy then J-pouch creation one year later. One month following J-pouch creation, she developed severe Crohn’s-like enteritis with CT showing narrowing at the distal duodenum. Push enteroscopy revealed diffuse inflammation and superficial ulcerations with biopsies showing active duodenitis without evidence of chronicity or granuloma. A follow-up push enteroscopy in December 2023 revealed severe duodenal inflammation with complete loss of normal mucosa, cobblestoning and deep ulcers. Biopsies showed chronic inflammation and ulceration. She was ultimately diagnosed with Crohn’s-like enteritis of the upper gastrointestinal tract, which differs from previous reports as all prior PCE cases have been in patients with a primary diagnosis of UC. She was effectively treated with corticosteroids and exclusive enteral nutrition (EEN) for induction of remission, and remains in clinical remission on Upadacitinib monotherapy as of May 2024.
Discussion: The pathogenesis of PCE is unknown and although most patients are treated with corticosteroids for inducing remission, there is no agreement on the choice of long-term therapy. Various maintenance therapies have been used to date including azathioprine, tacrolimus and infliximab. In this case, the patient was effectively treated with corticosteroids, EEN and Upadacitinib. Overall, this may represent a distinctive form of severe Crohn’s-like enteritis post colectomy in UC, a spectrum of PCE, or progression of UC to CD following colectomy. While more research is necessary to establish diagnostic clarity and treatment guidelines, treatment with corticosteroids, EEN and Upadacitinib may be safe and effective therapies for severe Crohn’s-like enteritis post colectomy.
Disclosures:
Leona Chan, MD1, Eric Lam, MD,2, Yvette Leung, MD3, Jeremy Liu Chen Kiow, MD2. P2728 - Upadacitinib for Severe Crohn's-Like Enteritis Following Colectomy for Ulcerative Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Alberta, Edmonton, AB, Canada; 2University of British Columbia, Vancouver, BC, Canada; 3University of British Columbia, IBD Centre of BC, Vancouver, BC, Canada
Introduction: Ulcerative colitis (UC) is an inflammatory condition typically confined to the rectum and colon. Occasionally, the small bowel can be affected with multiple well-described variants including backwash ileitis, post-colectomy pouchitis and enteritis in UC. In recent decades, several case reports have described a distinctive form of fulminant enteritis following colectomy in UC patients, known as postcolectomy enteritis (PCE), requiring corticosteroid induction and immunosuppressive maintenance therapy. However, the pathogenesis of PCE, its association with UC or Crohn’s Disease (CD), and optimal therapy remains unclear.
Case Description/Methods: We present a 23-year-old female initially diagnosed with UC in October 2022 based on imaging, endoscopic and pathology findings, who underwent total colectomy then J-pouch creation one year later. One month following J-pouch creation, she developed severe Crohn’s-like enteritis with CT showing narrowing at the distal duodenum. Push enteroscopy revealed diffuse inflammation and superficial ulcerations with biopsies showing active duodenitis without evidence of chronicity or granuloma. A follow-up push enteroscopy in December 2023 revealed severe duodenal inflammation with complete loss of normal mucosa, cobblestoning and deep ulcers. Biopsies showed chronic inflammation and ulceration. She was ultimately diagnosed with Crohn’s-like enteritis of the upper gastrointestinal tract, which differs from previous reports as all prior PCE cases have been in patients with a primary diagnosis of UC. She was effectively treated with corticosteroids and exclusive enteral nutrition (EEN) for induction of remission, and remains in clinical remission on Upadacitinib monotherapy as of May 2024.
Discussion: The pathogenesis of PCE is unknown and although most patients are treated with corticosteroids for inducing remission, there is no agreement on the choice of long-term therapy. Various maintenance therapies have been used to date including azathioprine, tacrolimus and infliximab. In this case, the patient was effectively treated with corticosteroids, EEN and Upadacitinib. Overall, this may represent a distinctive form of severe Crohn’s-like enteritis post colectomy in UC, a spectrum of PCE, or progression of UC to CD following colectomy. While more research is necessary to establish diagnostic clarity and treatment guidelines, treatment with corticosteroids, EEN and Upadacitinib may be safe and effective therapies for severe Crohn’s-like enteritis post colectomy.
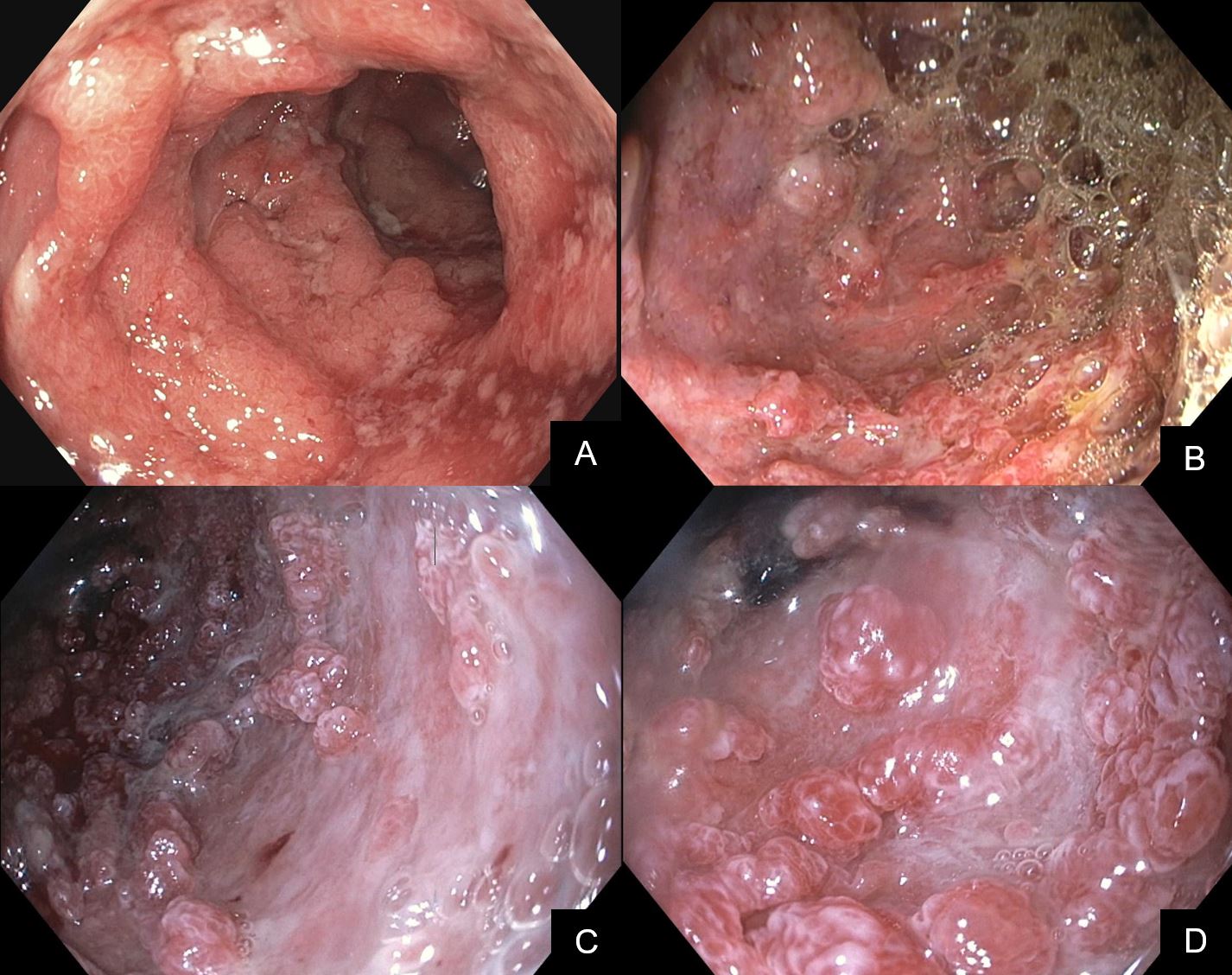
Figure: Figure 1. Endoscopic images from (A) Diagnostic colonoscopy in October 2022 showing severe continuous colitis (Mayo 3) with deep ulcerations to the extent of exam, (B) Push enteroscopy in November 2023 following J-pouch creation showing diffuse inflammation with superficial ulcerations involving the stomach and duodenum, (C,D) Follow-up push enteroscopy in December 2023 showing severe inflammation in the duodenum with complete loss of normal mucosa, cobblestoning and deep ulcers.
Disclosures:
Leona Chan indicated no relevant financial relationships.
Eric Lam indicated no relevant financial relationships.
Yvette Leung: Abbvie – Advisory Committee/Board Member, Speakers Bureau. Amgen – Advisory Committee/Board Member, Speakers Bureau. BMS – Advisory Committee/Board Member, Speakers Bureau. Eli Lilly – Advisory Committee/Board Member, Speakers Bureau. Janssen – Advisory Committee/Board Member, Speakers Bureau. Organon – Advisory Committee/Board Member, Speakers Bureau. Pfizer – Advisory Committee/Board Member, Speakers Bureau. Takeda – Advisory Committee/Board Member, Speakers Bureau.
Jeremy Liu Chen Kiow indicated no relevant financial relationships.
Leona Chan, MD1, Eric Lam, MD,2, Yvette Leung, MD3, Jeremy Liu Chen Kiow, MD2. P2728 - Upadacitinib for Severe Crohn's-Like Enteritis Following Colectomy for Ulcerative Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
