Monday Poster Session
Category: IBD
P2636 - Unveiling the Postpartum Peril: Assessing Inflammatory Bowel Disease's Impact on Hospital Readmissions
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Sanket Basida, MD
University of Missouri School of Medicine
Columbia, MO
Presenting Author(s)
Sanket Basida, MD1, Neel Vora, MBBS2, Muhammad Nadeem. Yousaf, MD3, Dushyant S. Dahiya, MD4, Bhanu Siva Mohan Pinnam, MD5, Madhav Changela, MD6, Ebubekir Daglilar, MD7
1University of Missouri School of Medicine, Columbia, MO; 2B.J. Medical College, Rajkot, Gujarat, India; 3University of Missouri Health Care, Columbia, MO; 4The University of Kansas School of Medicine, Kansas City, KS; 5John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 6One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 7Charleston Area Medical Center, Charleston, WV
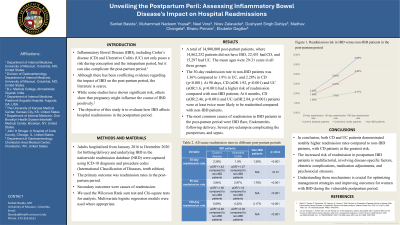
Introduction: Inflammatory Bowel Disease (IBD), including Crohn’s disease (CD) and Ulcerative Colitis (UC) not only poses a risk during conception and the intrapartum period, but it can also complicate the post-partum period. Although there has been conflicting evidence regarding the impact of IBD on the post-partum period, the literature is scarce. While some studies have shown significant risk, others show that pregnancy might influence the course of IBD positively. The objective of this study is to evaluate how IBD affects hospital readmissions in the postpartum period
Methods: Adults hospitalized from January 2016 to December 2020 for birthing/delivery and underlying IBD in the nationwide readmission database (NRD) were captured using ICD-10 diagnosis and procedure codes (International Classification of Diseases, tenth edition). The primary outcome was readmission rates in the post-partum period. Secondary outcomes were causes of readmission. We used the Wilcoxon Rank sum test and Chi-square tests for analysis. Multivariate logistic regression models were used where appropriate
Results: A total of 14,900,000 post-partum patients, where 14,862,252 patients did not have IBD, 22,451 had CD, and 15,297 had UC. The mean ages were 29-31 years in all three groups. The 30-day readmission rate in non-IBD patients was 1.36% compared to 1.9% in UC, and 2.28% in CD (p< 0.001). At 90 days, CD (aOR:1.92, p< 0.001) and UC (aOR:1.6, p< 0.001) had a higher risk of readmission compared with non-IBD patients. At 6 months, CD (aOR:2.46, p< 0.001) and UC (aOR:2.04, p< 0.001) patients were at least twice more likely to be readmitted compared with non-IBD patients. The most common causes of readmission in IBD patients in the post-partum period were IBD flare, Endometritis following delivery, Severe pre-eclampsia complicating the puerperium, and sepsis.
Discussion: In conclusion, both CD and UC patients demonstrated notably higher readmission rates compared to non-IBD patients, with CD patients at the greatest risk. The increased risk of readmission in postpartum IBD patients is multifactorial, involving disease-specific factors, obstetric complications, medication adjustments, and psychosocial stressors. Understanding these mechanisms is crucial for optimizing management strategies and improving outcomes for women with IBD during the vulnerable postpartum period.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sanket Basida, MD1, Neel Vora, MBBS2, Muhammad Nadeem. Yousaf, MD3, Dushyant S. Dahiya, MD4, Bhanu Siva Mohan Pinnam, MD5, Madhav Changela, MD6, Ebubekir Daglilar, MD7. P2636 - Unveiling the Postpartum Peril: Assessing Inflammatory Bowel Disease's Impact on Hospital Readmissions, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Missouri School of Medicine, Columbia, MO; 2B.J. Medical College, Rajkot, Gujarat, India; 3University of Missouri Health Care, Columbia, MO; 4The University of Kansas School of Medicine, Kansas City, KS; 5John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 6One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 7Charleston Area Medical Center, Charleston, WV
Introduction: Inflammatory Bowel Disease (IBD), including Crohn’s disease (CD) and Ulcerative Colitis (UC) not only poses a risk during conception and the intrapartum period, but it can also complicate the post-partum period. Although there has been conflicting evidence regarding the impact of IBD on the post-partum period, the literature is scarce. While some studies have shown significant risk, others show that pregnancy might influence the course of IBD positively. The objective of this study is to evaluate how IBD affects hospital readmissions in the postpartum period
Methods: Adults hospitalized from January 2016 to December 2020 for birthing/delivery and underlying IBD in the nationwide readmission database (NRD) were captured using ICD-10 diagnosis and procedure codes (International Classification of Diseases, tenth edition). The primary outcome was readmission rates in the post-partum period. Secondary outcomes were causes of readmission. We used the Wilcoxon Rank sum test and Chi-square tests for analysis. Multivariate logistic regression models were used where appropriate
Results: A total of 14,900,000 post-partum patients, where 14,862,252 patients did not have IBD, 22,451 had CD, and 15,297 had UC. The mean ages were 29-31 years in all three groups. The 30-day readmission rate in non-IBD patients was 1.36% compared to 1.9% in UC, and 2.28% in CD (p< 0.001). At 90 days, CD (aOR:1.92, p< 0.001) and UC (aOR:1.6, p< 0.001) had a higher risk of readmission compared with non-IBD patients. At 6 months, CD (aOR:2.46, p< 0.001) and UC (aOR:2.04, p< 0.001) patients were at least twice more likely to be readmitted compared with non-IBD patients. The most common causes of readmission in IBD patients in the post-partum period were IBD flare, Endometritis following delivery, Severe pre-eclampsia complicating the puerperium, and sepsis.
Discussion: In conclusion, both CD and UC patients demonstrated notably higher readmission rates compared to non-IBD patients, with CD patients at the greatest risk. The increased risk of readmission in postpartum IBD patients is multifactorial, involving disease-specific factors, obstetric complications, medication adjustments, and psychosocial stressors. Understanding these mechanisms is crucial for optimizing management strategies and improving outcomes for women with IBD during the vulnerable postpartum period.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sanket Basida indicated no relevant financial relationships.
Neel Vora indicated no relevant financial relationships.
Muhammad Yousaf indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Bhanu Siva Mohan Pinnam indicated no relevant financial relationships.
Madhav Changela indicated no relevant financial relationships.
Ebubekir Daglilar indicated no relevant financial relationships.
Sanket Basida, MD1, Neel Vora, MBBS2, Muhammad Nadeem. Yousaf, MD3, Dushyant S. Dahiya, MD4, Bhanu Siva Mohan Pinnam, MD5, Madhav Changela, MD6, Ebubekir Daglilar, MD7. P2636 - Unveiling the Postpartum Peril: Assessing Inflammatory Bowel Disease's Impact on Hospital Readmissions, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
