Monday Poster Session
Category: IBD
P2637 - Opioid Prescriptions at Discharge From the Emergency Department or Hospital Are Associated With Several Poor Outcomes in Inflammatory Bowel Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- MC
Matthew Coates, MD, PhD
Penn State Health Milton S. Hershey Medical Center
Hershey, PA
Presenting Author(s)
Wes Heinle, MPH1, Eric Schaefer, MS1, Guodong Liu, PhD1, Matthew Coates, MD, PhD2
1Penn State College of Medicine, Hershey, PA; 2Penn State Health Milton S. Hershey Medical Center, Hershey, PA
Introduction: Pain is common in inflammatory bowel disease (IBD), and its management remains a significant challenge. Opioids are becoming more frequently used for this purpose, particularly in acute care settings, despite their associated risks. We undertook this study to evaluate clinical outcomes in IBD patients who had been prescribed opioids after being managed in an acute care setting.
Methods: Using the Merative MarketScan® claims database, we performed a retrospective analysis of adults with established IBD who visited an emergency department (ED) and/or were hospitalized between 2017-2021 and had not filled an opioid prescription within 6 months prior to the event. We identified whether a new opioid prescription was filled within 7 days of the ED/hospital discharge, and compared outcomes at 1, 3, and 6 months after the ED visit/hospitalization using logistic regression that accounted for key variables.
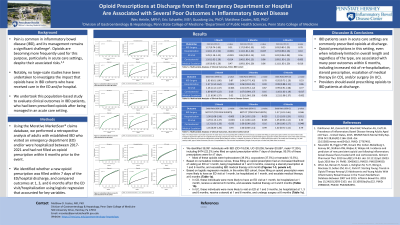
Results: We identified 38,091 individuals with IBD (CD=18,036, UC=20,055; female=20,887, male=17,204), including 8474 (22.2%) who filled an opioid prescription within 7 days of discharge. 95.0% of these prescriptions were for ≤7 days. Most of these opioids were hydrocodone (39.0%), oxycodone (37.5%) or tramadol (13.5%). Based on logistic regression models, those filling an opioid prescription had an increased likelihood of visiting an ED at 1 month (odds ratio [OR]=1.34, 95% confidence interval [CI]:1.18-1.42, p< 0.001), being hospitalized at 1 (OR=1.34, CI:1.17-1.52, p< 0.001) and 3 months (OR=1.11, CI:1.01-1.22, p=0.03), receiving a steroid prescription at 1 (OR=1.10, CI:1.02-1.20, p=0.01) and 6 months (OR=1.09, CI:1.03-1.15, p=0.003), and escalating IBD medical therapy at 6 months (OR=1.11, CI:1.02-1.20, p=0.02). In CD, those filling an opioid prescription were more likely to have an ED visit at 1 month, be hospitalized at 1 month, receive a steroid at 6 months, and escalate medical therapy at 3 and 6 months (Table 1a). In UC, these individuals were more likely to visit an ED at 1 and 3 months, be hospitalized at 1, 3 and 6 months, receive a steroid at 1 and 6 months, and undergo surgery at 6 months (Table 1b).
Discussion: IBD patients in acute care settings are commonly prescribed opioids at discharge. Opioid prescriptions in this setting, even when relatively limited in overall length and regardless of the type, are associated with many poor outcomes within 6 months. Providers should avoid prescribing opioids to IBD patients at discharge.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Wes Heinle, MPH1, Eric Schaefer, MS1, Guodong Liu, PhD1, Matthew Coates, MD, PhD2. P2637 - Opioid Prescriptions at Discharge From the Emergency Department or Hospital Are Associated With Several Poor Outcomes in Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Penn State College of Medicine, Hershey, PA; 2Penn State Health Milton S. Hershey Medical Center, Hershey, PA
Introduction: Pain is common in inflammatory bowel disease (IBD), and its management remains a significant challenge. Opioids are becoming more frequently used for this purpose, particularly in acute care settings, despite their associated risks. We undertook this study to evaluate clinical outcomes in IBD patients who had been prescribed opioids after being managed in an acute care setting.
Methods: Using the Merative MarketScan® claims database, we performed a retrospective analysis of adults with established IBD who visited an emergency department (ED) and/or were hospitalized between 2017-2021 and had not filled an opioid prescription within 6 months prior to the event. We identified whether a new opioid prescription was filled within 7 days of the ED/hospital discharge, and compared outcomes at 1, 3, and 6 months after the ED visit/hospitalization using logistic regression that accounted for key variables.
Results: We identified 38,091 individuals with IBD (CD=18,036, UC=20,055; female=20,887, male=17,204), including 8474 (22.2%) who filled an opioid prescription within 7 days of discharge. 95.0% of these prescriptions were for ≤7 days. Most of these opioids were hydrocodone (39.0%), oxycodone (37.5%) or tramadol (13.5%). Based on logistic regression models, those filling an opioid prescription had an increased likelihood of visiting an ED at 1 month (odds ratio [OR]=1.34, 95% confidence interval [CI]:1.18-1.42, p< 0.001), being hospitalized at 1 (OR=1.34, CI:1.17-1.52, p< 0.001) and 3 months (OR=1.11, CI:1.01-1.22, p=0.03), receiving a steroid prescription at 1 (OR=1.10, CI:1.02-1.20, p=0.01) and 6 months (OR=1.09, CI:1.03-1.15, p=0.003), and escalating IBD medical therapy at 6 months (OR=1.11, CI:1.02-1.20, p=0.02). In CD, those filling an opioid prescription were more likely to have an ED visit at 1 month, be hospitalized at 1 month, receive a steroid at 6 months, and escalate medical therapy at 3 and 6 months (Table 1a). In UC, these individuals were more likely to visit an ED at 1 and 3 months, be hospitalized at 1, 3 and 6 months, receive a steroid at 1 and 6 months, and undergo surgery at 6 months (Table 1b).
Discussion: IBD patients in acute care settings are commonly prescribed opioids at discharge. Opioid prescriptions in this setting, even when relatively limited in overall length and regardless of the type, are associated with many poor outcomes within 6 months. Providers should avoid prescribing opioids to IBD patients at discharge.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Wes Heinle indicated no relevant financial relationships.
Eric Schaefer indicated no relevant financial relationships.
Guodong Liu indicated no relevant financial relationships.
Matthew Coates indicated no relevant financial relationships.
Wes Heinle, MPH1, Eric Schaefer, MS1, Guodong Liu, PhD1, Matthew Coates, MD, PhD2. P2637 - Opioid Prescriptions at Discharge From the Emergency Department or Hospital Are Associated With Several Poor Outcomes in Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
