Monday Poster Session
Category: IBD
P2639 - Type 2 Diabetes and Risk of Incident Inflammatory Bowel Disease in U.S. Adults
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MS
Miyabi Saito, MD
Massachusetts General Hospital, Harvard Medical School
Boston, MA
Presenting Author(s)
Miyabi Saito, MD1, Emily W.. Lopes, MD, MPH2, Chun-Han Lo, MD3, Ashwin Ananthakrishnan, MBBS, MPH2, Kristin Burke, MD, MPH2, James M.. Richter, MD4, Andrew Chan, MD, MPH1, Hamed Khalili, MD, MPH1
1Massachusetts General Hospital, Harvard Medical School, Boston, MA; 2Massachusetts General Hospital, Boston, MA; 3Harvard T.H. Chan School of Public Health, Boston, MA; 4Boston, MA
Introduction: Sucrose and sugary beverages increase risk for inflammatory bowel disease (IBD). Impaired glucose control may also contribute to altered gut microbiota and a pro-inflammatory state. Type 1 diabetes mellitus (T1DM) increases risk for IBD, likely due to shared autoimmune factors. Here, we explored the relationship between type 2 DM (T2DM) and risk of incident Crohn’s disease (CD) and ulcerative colitis (UC).
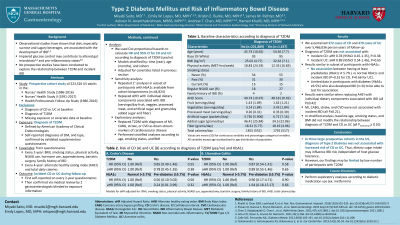
Methods: We conducted a prospective study of 223,526 US adults (mean age=45) from the Nurses’ Health study (NHS;1986-2016), NHSII (1991-2017), and Health Professionals Follow-up study (HPFS; 1986-2016). Covariate and dietary data were collected via questionnaires every 2- and 4-years, respectively. We excluded those with IBD or T1DM at baseline. Self-reported cases of DM were confirmed by validated supplementary questionnaires that utilized standard cutoffs for DM (fasting glucose ≥7.0 mmol/L, random glucose or ≥2h oral glucose tolerance test ≥11.1 mmol/L, or hemoglobin A1c ≥6.5%). Self-reported cases of IBD were confirmed via medical record review by two gastroenterologists. We used Cox proportional hazard models to estimate multivariable-adjusted hazard ratios (aHR) and 95% confidence intervals (CI) for CD and UC according to diagnosis of T2DM, adjusting for age, cohort, body mass index, family history of IBD, smoking, caloric intake, alternate healthy eating index (AHEI), physical activity, appendectomy, bariatric surgery, and non-steroidal anti-inflammatory use.
Results: We documented 372 CD and 479 UC cases over 5,466,084 person-years of follow up. Diagnosis of T2DM was not associated with incident CD or UC (P=0.54 and 0.58, respectively). Compared to participants without T2DM, the aHR for those with T2DM was 0.77 (95% CI 0.45-1.34) for CD and 0.89 (95% CI 0.55-1.46) for UC. Results were similar when replacing AHEI with dietary components associated with IBD (servings/day fruit, vegetables, processed meat, and artificial sugar and grams/day sugar and fiber; all P≥0.37). History of myocardial infarction, stroke, and coronary artery disease also were not associated with incident IBD (all P≥0.21).
Discussion: T2DM was not associated with risk of IBD in 3 large cohorts. Dietary sugar intake may therefore increase IBD risk independent of host glucose tolerance. However, our findings may not apply to younger populations, who experience higher rates of IBD. Further studies examining glucose control as measured by hemoglobin A1c and in younger cohorts are needed.
Disclosures:
Miyabi Saito, MD1, Emily W.. Lopes, MD, MPH2, Chun-Han Lo, MD3, Ashwin Ananthakrishnan, MBBS, MPH2, Kristin Burke, MD, MPH2, James M.. Richter, MD4, Andrew Chan, MD, MPH1, Hamed Khalili, MD, MPH1. P2639 - Type 2 Diabetes and Risk of Incident Inflammatory Bowel Disease in U.S. Adults, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Massachusetts General Hospital, Harvard Medical School, Boston, MA; 2Massachusetts General Hospital, Boston, MA; 3Harvard T.H. Chan School of Public Health, Boston, MA; 4Boston, MA
Introduction: Sucrose and sugary beverages increase risk for inflammatory bowel disease (IBD). Impaired glucose control may also contribute to altered gut microbiota and a pro-inflammatory state. Type 1 diabetes mellitus (T1DM) increases risk for IBD, likely due to shared autoimmune factors. Here, we explored the relationship between type 2 DM (T2DM) and risk of incident Crohn’s disease (CD) and ulcerative colitis (UC).
Methods: We conducted a prospective study of 223,526 US adults (mean age=45) from the Nurses’ Health study (NHS;1986-2016), NHSII (1991-2017), and Health Professionals Follow-up study (HPFS; 1986-2016). Covariate and dietary data were collected via questionnaires every 2- and 4-years, respectively. We excluded those with IBD or T1DM at baseline. Self-reported cases of DM were confirmed by validated supplementary questionnaires that utilized standard cutoffs for DM (fasting glucose ≥7.0 mmol/L, random glucose or ≥2h oral glucose tolerance test ≥11.1 mmol/L, or hemoglobin A1c ≥6.5%). Self-reported cases of IBD were confirmed via medical record review by two gastroenterologists. We used Cox proportional hazard models to estimate multivariable-adjusted hazard ratios (aHR) and 95% confidence intervals (CI) for CD and UC according to diagnosis of T2DM, adjusting for age, cohort, body mass index, family history of IBD, smoking, caloric intake, alternate healthy eating index (AHEI), physical activity, appendectomy, bariatric surgery, and non-steroidal anti-inflammatory use.
Results: We documented 372 CD and 479 UC cases over 5,466,084 person-years of follow up. Diagnosis of T2DM was not associated with incident CD or UC (P=0.54 and 0.58, respectively). Compared to participants without T2DM, the aHR for those with T2DM was 0.77 (95% CI 0.45-1.34) for CD and 0.89 (95% CI 0.55-1.46) for UC. Results were similar when replacing AHEI with dietary components associated with IBD (servings/day fruit, vegetables, processed meat, and artificial sugar and grams/day sugar and fiber; all P≥0.37). History of myocardial infarction, stroke, and coronary artery disease also were not associated with incident IBD (all P≥0.21).
Discussion: T2DM was not associated with risk of IBD in 3 large cohorts. Dietary sugar intake may therefore increase IBD risk independent of host glucose tolerance. However, our findings may not apply to younger populations, who experience higher rates of IBD. Further studies examining glucose control as measured by hemoglobin A1c and in younger cohorts are needed.
Disclosures:
Miyabi Saito indicated no relevant financial relationships.
Emily Lopes: .
Chun-Han Lo indicated no relevant financial relationships.
Ashwin Ananthakrishnan: Geneoscopy – Advisor or Review Panel Member.
Kristin Burke: Bristol Myers Squibb – Advisory Committee/Board Member.
James Richter indicated no relevant financial relationships.
Andrew Chan: Bayer Pharma AG – Consultant. Boehringer Ingelheim – Consultant. Pfizer – Consultant.
Hamed Khalili: Aditium Bio – Consultant. Vivante Health – Advisory Committee/Board Member.
Miyabi Saito, MD1, Emily W.. Lopes, MD, MPH2, Chun-Han Lo, MD3, Ashwin Ananthakrishnan, MBBS, MPH2, Kristin Burke, MD, MPH2, James M.. Richter, MD4, Andrew Chan, MD, MPH1, Hamed Khalili, MD, MPH1. P2639 - Type 2 Diabetes and Risk of Incident Inflammatory Bowel Disease in U.S. Adults, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
