Monday Poster Session
Category: IBD
P2652 - Monthly Variations in IBD Hospitalizations in Patients With and Without Comorbid Anxiety or Depression
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MS
Matt Sumethasorn, MD
Keck School of Medicine of the University of Southern California
Los Angeles, CA
Presenting Author(s)
Matt Sumethasorn, MD1, Sarah Razon, BS1, Patrick Chang, MD2, Sarah Sheibani, MD1, Damie Odufalu, MD1, Cynthia Cherfane, MD1, Jennifer L. Dodge, MPH1, Bing Zhang, MD1
1Keck School of Medicine of the University of Southern California, Los Angeles, CA; 2University of Southern California, Los Angeles, CA
Introduction: Prior studies have shown conflicting data regarding the seasonal variation of IBD exacerbations. This is likely due to the inability to account for the unknown various environmental factors that are thought to influence the pathogenesis of IBD. Psychological stress is a known environmental trigger for IBD flares, and patients with IBD have higher rates of developing anxiety and depression. In this study we looked at monthly variations in IBD admissions in those with and without comorbid anxiety or depression.
Methods: Using the National Inpatient Sample database from 2016-2019, we identified adult hospitalization (≥18 years) with a primary diagnosis of IBD (including Crohn’s Disease and Ulcerative Colitis, ICD-10 K50-51), and separately, adult hospitalizations with a primary diagnosis of IBD with concurrent depression (ICD F32-F33) and/or anxiety (ICD-10 F41). The primary outcome was monthly hospitalization rate per 100,000 hospitalizations estimated as weighted means to account for the complex survey design and generate nationally representative estimates. Differences in monthly hospitalization rates were estimated using linear regression. To account for multiple testing, we used a Bonferroni adjusted significance level of 0.0042 (0.05/12 months).
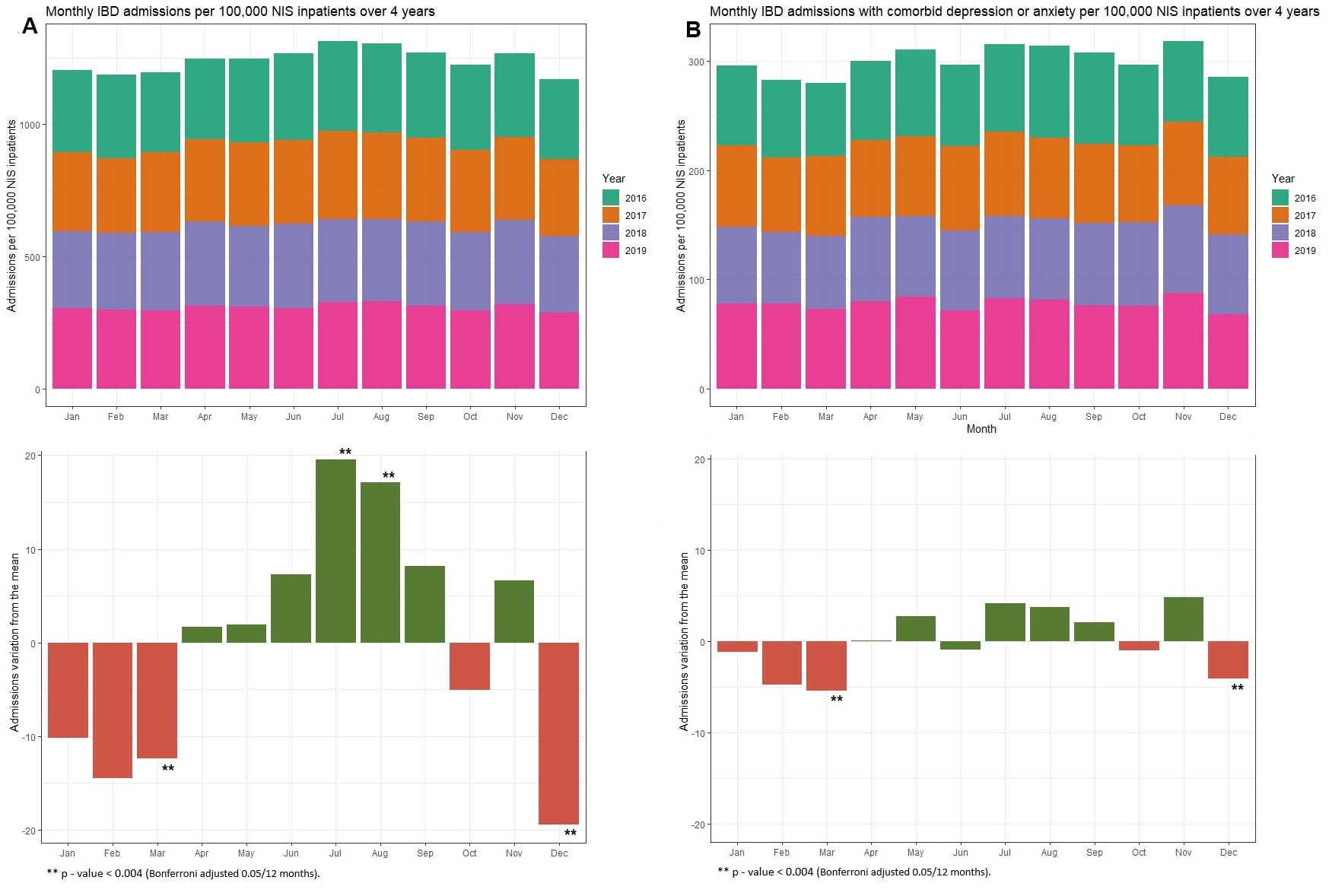
Results: IBD hospitalizations peaked in July, with an increase of 19.6 more monthly hospitalizations per 100,000 when compared to the average (p < 0.001; Fig. 1A, Table 1A). This was followed closely by August, with an increase of 17.1 admissions per 100,000. Conversely, the lowest hospitalization rates occurred in the winter, with December having 19.4 fewer hospitalizations per 100,000 (p < 0.001). Among IBD patients with depression and/or anxiety, hospitalizations were lower by 5.5 in March and 4.1 in December. (p = 0.002; Fig. 1B, Table 1B); there was no statistically significant increase in any months.
Discussion: Our study demonstrates significantly lower hospitalization rates in March and December among IBD patients, both with and without anxiety and/or depression. Surprisingly, hospitalization rates among IBD patients without anxiety and/or depression rose in the summer months and nadired in December, suggesting environmental cues which may influence IBD hospitalizations compared to other non-IBD hospitalizations. Future research is needed to identify modifiable risk factors for IBD hospitalization rates during the summer months.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Matt Sumethasorn, MD1, Sarah Razon, BS1, Patrick Chang, MD2, Sarah Sheibani, MD1, Damie Odufalu, MD1, Cynthia Cherfane, MD1, Jennifer L. Dodge, MPH1, Bing Zhang, MD1. P2652 - Monthly Variations in IBD Hospitalizations in Patients With and Without Comorbid Anxiety or Depression, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Keck School of Medicine of the University of Southern California, Los Angeles, CA; 2University of Southern California, Los Angeles, CA
Introduction: Prior studies have shown conflicting data regarding the seasonal variation of IBD exacerbations. This is likely due to the inability to account for the unknown various environmental factors that are thought to influence the pathogenesis of IBD. Psychological stress is a known environmental trigger for IBD flares, and patients with IBD have higher rates of developing anxiety and depression. In this study we looked at monthly variations in IBD admissions in those with and without comorbid anxiety or depression.
Methods: Using the National Inpatient Sample database from 2016-2019, we identified adult hospitalization (≥18 years) with a primary diagnosis of IBD (including Crohn’s Disease and Ulcerative Colitis, ICD-10 K50-51), and separately, adult hospitalizations with a primary diagnosis of IBD with concurrent depression (ICD F32-F33) and/or anxiety (ICD-10 F41). The primary outcome was monthly hospitalization rate per 100,000 hospitalizations estimated as weighted means to account for the complex survey design and generate nationally representative estimates. Differences in monthly hospitalization rates were estimated using linear regression. To account for multiple testing, we used a Bonferroni adjusted significance level of 0.0042 (0.05/12 months).
Results: IBD hospitalizations peaked in July, with an increase of 19.6 more monthly hospitalizations per 100,000 when compared to the average (p < 0.001; Fig. 1A, Table 1A). This was followed closely by August, with an increase of 17.1 admissions per 100,000. Conversely, the lowest hospitalization rates occurred in the winter, with December having 19.4 fewer hospitalizations per 100,000 (p < 0.001). Among IBD patients with depression and/or anxiety, hospitalizations were lower by 5.5 in March and 4.1 in December. (p = 0.002; Fig. 1B, Table 1B); there was no statistically significant increase in any months.
Discussion: Our study demonstrates significantly lower hospitalization rates in March and December among IBD patients, both with and without anxiety and/or depression. Surprisingly, hospitalization rates among IBD patients without anxiety and/or depression rose in the summer months and nadired in December, suggesting environmental cues which may influence IBD hospitalizations compared to other non-IBD hospitalizations. Future research is needed to identify modifiable risk factors for IBD hospitalization rates during the summer months.
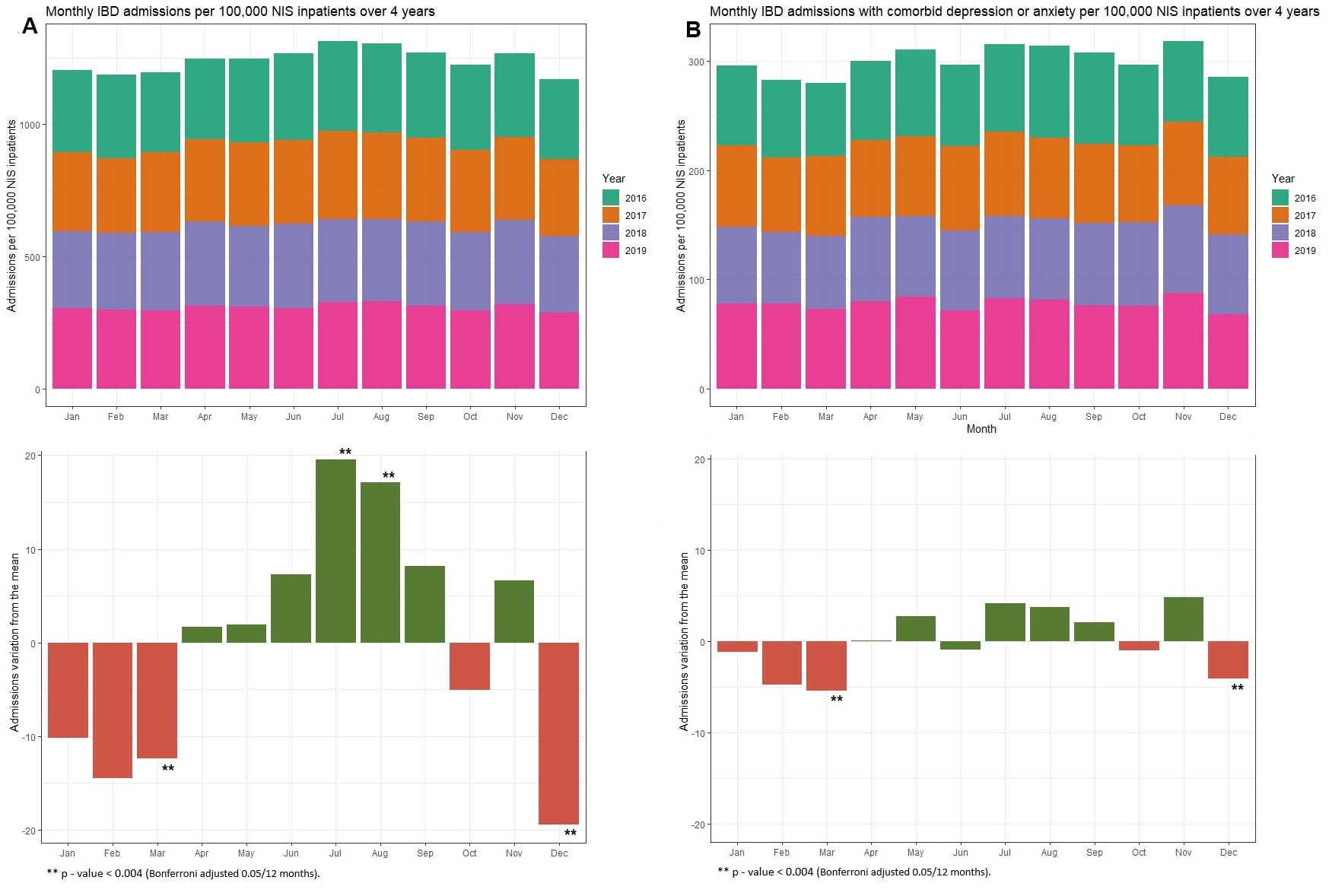
Figure: Figure 1: A) Above: IBD admissions per 100,000 total NIS inpatient by month from 2016 to 2019. Below: Differences in monthly hospitalization rates estimated by linear regression when compared to the average. B) Above: IBD admissions with comorbid depression or anxiety per 100,000 total NIS inpatient by month.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Matt Sumethasorn indicated no relevant financial relationships.
Sarah Razon indicated no relevant financial relationships.
Patrick Chang indicated no relevant financial relationships.
Sarah Sheibani indicated no relevant financial relationships.
Damie Odufalu indicated no relevant financial relationships.
Cynthia Cherfane indicated no relevant financial relationships.
Jennifer Dodge indicated no relevant financial relationships.
Bing Zhang indicated no relevant financial relationships.
Matt Sumethasorn, MD1, Sarah Razon, BS1, Patrick Chang, MD2, Sarah Sheibani, MD1, Damie Odufalu, MD1, Cynthia Cherfane, MD1, Jennifer L. Dodge, MPH1, Bing Zhang, MD1. P2652 - Monthly Variations in IBD Hospitalizations in Patients With and Without Comorbid Anxiety or Depression, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
