Monday Poster Session
Category: IBD
P2654 - The Impact of Disease Status After Biologic Induction Therapy on Long-Term Outcomes in Persons With Crohn’s Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Gurmun S. Brar, MD
University of Toronto
Toronto, ON, Canada
Presenting Author(s)
Gurmun S. Brar, MD1, Parul Tandon, DO, PhD2, Muzzafar Haque, MD3, Nazish K. Butt, MBBS, MS4, Myrlene Sanon, MPH5, Dominik H R. Naessens, PhD, PharmD, MBA6, Eneda Pone, MBA, BSc7, Laura E. Targownik, MD, MSHS1
1University of Toronto, Toronto, ON, Canada; 2University Health Network, Toronto, ON, Canada; 3University of Saskatchewan, Regina, SK, Canada; 4Sinai Hospital, Toronto, ON, Canada; 5Janssen Global Services, Horsham, PA; 6Janssen Pharmaceutica NV, Beerse, Antwerpen, Belgium; 7Janssen, Toronto, ON, Canada
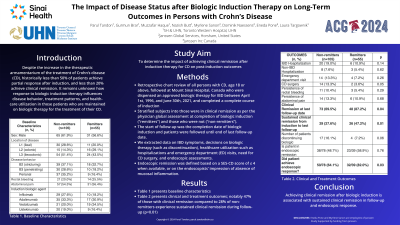
Introduction: Historically, less than 20% of patients with Crohn’s disease (CD) achieve clinical remission after induction with biologic therapy. It is unknown how response to biologic induction influences disease behavior, treatment patterns, and healthcare utilization for patients maintained on biologic therapy long-term. We aimed to elucidate the impact of achieving clinical remission after biologic induction on long-term disease outcomes.
Methods: We conducted a retrospective cohort study including all patients with CD who completed biologic induction at Mount Sinai Hospital, Canada before June 30, 2021. Patients were stratified by response to biologic induction as per physician global assessment as remitters (clinical remission) and non-remitters (partial or no-response). We extracted data on disease activity (symptoms, biochemistry, endoscopy, imaging), IBD-related complications, IBD-related healthcare utilization (ED, hospitalization, surgery), and changes to pharmacotherapy until end of follow-up. Endoscopic remission was defined as SES-CD score less than 4 or based on the endoscopist's impression.
Results: Of the 160 patients included, 35.6%, 25.0%, and 28.9% had stricturing, penetrating, and perianal disease respectively, with 34.3% having a history of CD surgery. Index biologic included infliximab (24.4%), adalimumab (32.5%), vedolizumab (25.0%), and ustekinumab (11.9%). After biologic induction, 34.4% and 65.6% of patients were stratified as remitters and non-remitters respectively. Remitters were less likely to have upper gastrointestinal CD (3.6% vs. 10.5%), penetrating complications (18.2% vs. 28.6%), and perianal disease (16.4% vs. 35.2%) at biologic start. Compared to non-remitters, remitters were more likely to be in clinical remission throughout follow-up (47.2% vs. 27.6%, p=0.01) and in clinical remission at last follow-up (87.2% vs. 69.5%, p=0.04). Remitters were less likely to undergo CD-related bowel resection (3.6% vs. 13.3%, p=0.05) or discontinue index biologic (7.2% vs. 16.1%, p=0.06). There appeared to be no significant difference in IBD hospitalizations (10.9% vs. 19.0%, p=0.14) or ED visits (7.2% vs. 13.3%, p=0.26). There was no difference in rates of ulcer persistence (51.6% vs. 53.5%, p=0.63) or achievement of endoscopic remission (58.9% vs. 48.7%, p=0.76) between remitters and non-remitters.
Discussion: Achieving clinical remission after biologic induction is associated with sustained clinical remission and reduced likelihood of subsequent CD-related bowel resection.
Disclosures:
Gurmun S. Brar, MD1, Parul Tandon, DO, PhD2, Muzzafar Haque, MD3, Nazish K. Butt, MBBS, MS4, Myrlene Sanon, MPH5, Dominik H R. Naessens, PhD, PharmD, MBA6, Eneda Pone, MBA, BSc7, Laura E. Targownik, MD, MSHS1. P2654 - The Impact of Disease Status After Biologic Induction Therapy on Long-Term Outcomes in Persons With Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Toronto, Toronto, ON, Canada; 2University Health Network, Toronto, ON, Canada; 3University of Saskatchewan, Regina, SK, Canada; 4Sinai Hospital, Toronto, ON, Canada; 5Janssen Global Services, Horsham, PA; 6Janssen Pharmaceutica NV, Beerse, Antwerpen, Belgium; 7Janssen, Toronto, ON, Canada
Introduction: Historically, less than 20% of patients with Crohn’s disease (CD) achieve clinical remission after induction with biologic therapy. It is unknown how response to biologic induction influences disease behavior, treatment patterns, and healthcare utilization for patients maintained on biologic therapy long-term. We aimed to elucidate the impact of achieving clinical remission after biologic induction on long-term disease outcomes.
Methods: We conducted a retrospective cohort study including all patients with CD who completed biologic induction at Mount Sinai Hospital, Canada before June 30, 2021. Patients were stratified by response to biologic induction as per physician global assessment as remitters (clinical remission) and non-remitters (partial or no-response). We extracted data on disease activity (symptoms, biochemistry, endoscopy, imaging), IBD-related complications, IBD-related healthcare utilization (ED, hospitalization, surgery), and changes to pharmacotherapy until end of follow-up. Endoscopic remission was defined as SES-CD score less than 4 or based on the endoscopist's impression.
Results: Of the 160 patients included, 35.6%, 25.0%, and 28.9% had stricturing, penetrating, and perianal disease respectively, with 34.3% having a history of CD surgery. Index biologic included infliximab (24.4%), adalimumab (32.5%), vedolizumab (25.0%), and ustekinumab (11.9%). After biologic induction, 34.4% and 65.6% of patients were stratified as remitters and non-remitters respectively. Remitters were less likely to have upper gastrointestinal CD (3.6% vs. 10.5%), penetrating complications (18.2% vs. 28.6%), and perianal disease (16.4% vs. 35.2%) at biologic start. Compared to non-remitters, remitters were more likely to be in clinical remission throughout follow-up (47.2% vs. 27.6%, p=0.01) and in clinical remission at last follow-up (87.2% vs. 69.5%, p=0.04). Remitters were less likely to undergo CD-related bowel resection (3.6% vs. 13.3%, p=0.05) or discontinue index biologic (7.2% vs. 16.1%, p=0.06). There appeared to be no significant difference in IBD hospitalizations (10.9% vs. 19.0%, p=0.14) or ED visits (7.2% vs. 13.3%, p=0.26). There was no difference in rates of ulcer persistence (51.6% vs. 53.5%, p=0.63) or achievement of endoscopic remission (58.9% vs. 48.7%, p=0.76) between remitters and non-remitters.
Discussion: Achieving clinical remission after biologic induction is associated with sustained clinical remission and reduced likelihood of subsequent CD-related bowel resection.
Disclosures:
Gurmun Brar indicated no relevant financial relationships.
Parul Tandon: Abbvie – Speakers Bureau. Janssen – Advisory Committee/Board Member. Takeda – Speakers Bureau.
Muzzafar Haque indicated no relevant financial relationships.
Nazish Butt indicated no relevant financial relationships.
Myrlene Sanon: Janssen Global Services – Employee, Stock-publicly held company(excluding mutual/index funds).
Dominik Naessens: Apotheek Naessens-Cleeren – Stock-privately held company. Johnson & Johnson – Employee, Stock Options, Stock-publicly held company(excluding mutual/index funds).
Eneda Pone indicated no relevant financial relationships.
Laura Targownik: Abbvie – Advisor or Review Panel Member. Amgen – Advisory Committee/Board Member. Celltrion – Advisory Committee/Board Member. Fresenius Kabi – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member, Consultant, Grant/Research Support. Lilly – Advisory Committee/Board Member, Grant/Research Support. Organon – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member, Grant/Research Support. Takeda – Advisory Committee/Board Member.
Gurmun S. Brar, MD1, Parul Tandon, DO, PhD2, Muzzafar Haque, MD3, Nazish K. Butt, MBBS, MS4, Myrlene Sanon, MPH5, Dominik H R. Naessens, PhD, PharmD, MBA6, Eneda Pone, MBA, BSc7, Laura E. Targownik, MD, MSHS1. P2654 - The Impact of Disease Status After Biologic Induction Therapy on Long-Term Outcomes in Persons With Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
