Monday Poster Session
Category: IBD
P2576 - Primary Sclerosing Cholangitis: Evaluating Colorectal Cancer Risk With and Without Concurrent Inflammatory Bowel Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpeg.jpg)
Tarek Odah, MD
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Tarek Odah, MD1, Abdelrahman Yakout, MD1, Aasma Shaukat, MD, MPH2, Fadi F. Francis, MD3, Nayantara Coelho-Prabhu, MD, FACG4, Rami Tfayli, MD1, Francis A. Farraye, MD, MSc1, Jana G. Hashash, MD, MSc1
1Mayo Clinic, Jacksonville, FL; 2NYU Langone Health, New York, NY; 3University of Pittsburgh, Pittsburgh, PA; 4Mayo Clinic, Rochester, MN
Introduction: Primary sclerosing cholangitis (PSC) is a chronic and progressive liver disease characterized by bile duct inflammation and subsequent cholestasis. Almost 80% of patients with PSC have inflammatory bowel disease (IBD), particularly ulcerative colitis (UC). Patients with both PSC and IBD are at an increased risk for colorectal cancer (CRC). Limited data exist regarding CRC risk among patients with PSC alone. Our study aims to compare the association of PSC with CRC in patients with and without concurrent IBD.
Methods: This is a multicenter retrospective study that included adult patients across our healthcare system with PSC who underwent a colonoscopy between January 2000 and May 2024. Data on patient demographics, family history, medical history including IBD and CRC history, and endoscopy findings were recorded. Statistical analysis included logistic regression and Fisher's exact test.
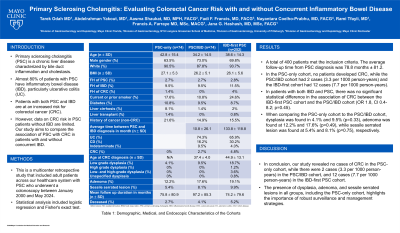
Results: A total of 400 patients met the inclusion criteria and were categorized into three cohorts: 74 in the PSC-only group, 74 in the PSC/IBD group (PSC preceding IBD or both diagnoses within three months), and 252 in the IBD-first group, diagnosed with IBD before PSC. The average follow-up time from PSC diagnosis was 78.8 months ± 81.2. Table 1 presents the demographics, medical, and endoscopic characteristics of the cohorts. In the PSC-only cohort, no patients developed CRC, while the PSC/IBD cohort had 2 cases (3.3 per 1000 person-years) and the IBD-first cohort had 12 cases (7.7 per 1000 person-years). In patients with both IBD and PSC, there was no significant statistical difference in the association of CRC between the IBD-first PSC cohort and the PSC/IBD cohort (OR 1.8, CI 0.4-8.2; p=0.45). When comparing the PSC-only cohort to the PSC/IBD cohort, dysplasia was found in 4.1% and 9.5% (p=0.33), adenoma was found at 12.2% and 17.6% (p=0.49), while sessile serrated lesion was found at 5.4% and 8.1% (p=0.75), respectively.
Discussion: In conclusion, our study revealed no cases of CRC in the PSC-only cohort, while there were 2 cases (3.3 per 1000 person-years) in the PSC/IBD cohort, and 12 cases (7.7 per 1000 person-years) in the IBD-first PSC cohort. The presence of dysplasia, adenoma, and sessile serrated lesions in all groups, including the PSC-only cohort, highlights the importance of robust surveillance and management strategies. Larger studies are required to establish optimal colonoscopy frequency in the PSC-only population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Tarek Odah, MD1, Abdelrahman Yakout, MD1, Aasma Shaukat, MD, MPH2, Fadi F. Francis, MD3, Nayantara Coelho-Prabhu, MD, FACG4, Rami Tfayli, MD1, Francis A. Farraye, MD, MSc1, Jana G. Hashash, MD, MSc1. P2576 - Primary Sclerosing Cholangitis: Evaluating Colorectal Cancer Risk With and Without Concurrent Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic, Jacksonville, FL; 2NYU Langone Health, New York, NY; 3University of Pittsburgh, Pittsburgh, PA; 4Mayo Clinic, Rochester, MN
Introduction: Primary sclerosing cholangitis (PSC) is a chronic and progressive liver disease characterized by bile duct inflammation and subsequent cholestasis. Almost 80% of patients with PSC have inflammatory bowel disease (IBD), particularly ulcerative colitis (UC). Patients with both PSC and IBD are at an increased risk for colorectal cancer (CRC). Limited data exist regarding CRC risk among patients with PSC alone. Our study aims to compare the association of PSC with CRC in patients with and without concurrent IBD.
Methods: This is a multicenter retrospective study that included adult patients across our healthcare system with PSC who underwent a colonoscopy between January 2000 and May 2024. Data on patient demographics, family history, medical history including IBD and CRC history, and endoscopy findings were recorded. Statistical analysis included logistic regression and Fisher's exact test.
Results: A total of 400 patients met the inclusion criteria and were categorized into three cohorts: 74 in the PSC-only group, 74 in the PSC/IBD group (PSC preceding IBD or both diagnoses within three months), and 252 in the IBD-first group, diagnosed with IBD before PSC. The average follow-up time from PSC diagnosis was 78.8 months ± 81.2. Table 1 presents the demographics, medical, and endoscopic characteristics of the cohorts. In the PSC-only cohort, no patients developed CRC, while the PSC/IBD cohort had 2 cases (3.3 per 1000 person-years) and the IBD-first cohort had 12 cases (7.7 per 1000 person-years). In patients with both IBD and PSC, there was no significant statistical difference in the association of CRC between the IBD-first PSC cohort and the PSC/IBD cohort (OR 1.8, CI 0.4-8.2; p=0.45). When comparing the PSC-only cohort to the PSC/IBD cohort, dysplasia was found in 4.1% and 9.5% (p=0.33), adenoma was found at 12.2% and 17.6% (p=0.49), while sessile serrated lesion was found at 5.4% and 8.1% (p=0.75), respectively.
Discussion: In conclusion, our study revealed no cases of CRC in the PSC-only cohort, while there were 2 cases (3.3 per 1000 person-years) in the PSC/IBD cohort, and 12 cases (7.7 per 1000 person-years) in the IBD-first PSC cohort. The presence of dysplasia, adenoma, and sessile serrated lesions in all groups, including the PSC-only cohort, highlights the importance of robust surveillance and management strategies. Larger studies are required to establish optimal colonoscopy frequency in the PSC-only population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Tarek Odah indicated no relevant financial relationships.
Abdelrahman Yakout indicated no relevant financial relationships.
Aasma Shaukat: iterative health; Freenome – Consultant.
Fadi Francis indicated no relevant financial relationships.
Nayantara Coelho-Prabhu: Iterative Health – Advisory Committee/Board Member.
Rami Tfayli indicated no relevant financial relationships.
Francis Farraye: AbbVie – Consultant. Avalo Therapeutics – Consultant. Bausch – Advisor or Review Panel Member. BMS – Consultant. Braintree Labs – Consultant. DSMB for Lilly. – Sits on. Fresenius Kabi – Consultant. GI Reviewers and IBD Educational Group – independent contractor. GSK, Iterative Health, Janssen, Pfizer, Pharmacosmos, Sandoz Immunology, Sebela and Viatris – Consultant.
Jana Hashash: Bristol Myers Squibb – Consultant.
Tarek Odah, MD1, Abdelrahman Yakout, MD1, Aasma Shaukat, MD, MPH2, Fadi F. Francis, MD3, Nayantara Coelho-Prabhu, MD, FACG4, Rami Tfayli, MD1, Francis A. Farraye, MD, MSc1, Jana G. Hashash, MD, MSc1. P2576 - Primary Sclerosing Cholangitis: Evaluating Colorectal Cancer Risk With and Without Concurrent Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
