Monday Poster Session
Category: IBD
P2582 - Examining the Relationship Between Transmural Response on MRE and Subjective Wellness Assessments in Small Bowel Crohn’s Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Brett D. Riederman, MD
Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital
St. Louis, MO
Presenting Author(s)
Brett D. Riederman, MD1, Richard Tsai, MD2, Chongliang Luo, PhD2, David Ballard, MD2, Parakkal Deepak, MBBS, MS3
1Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, MO; 2Washington University School of Medicine in St. Louis, St. Louis, MO; 3Washington University in St. Louis, St. Louis, MO
Introduction: In Crohn’s disease (CD), treatment goals have advanced over time with an objective of deep remission: absence of symptoms along with mucosal healing (MH) observed on ileocolonoscopy. In patients with small bowel CD, magnetic resonance enterography (MRE) has been used in place of ileocolonoscopy with a goal of assessing transmural response (TR). While TR may be a useful target in evaluating inflammation, it is not known whether this correlates with improvement in disease symptoms. We sought to determine if degree of inflammation on MRE is associated with subjective wellness measures.
Methods: We analyzed a cohort of 83 patients ages 18-80 with small bowel CD seen in Washington University IBD clinics. Initial visits took place from 2018 to 2021 with Week 0 Inflammatory Bowel Disease Disability Index (IBD-DI) and EQ-5D questionnaires completed at that time. This was repeated for those with visits at Week 52. Subjects also had a week 0 MRE which was completed within one year prior to initial clinic visit with week 52 MRE done within one month of week 52 visit. Each MRE was assessed by a specialized GI radiologist and scored using the simplified Magnetic Resonance Index of Activity (sMaRIA). Difference between Week 0 and 52 questionnaire scores was compared directly with associated sMaRIA values. Change in questionnaire scores was also assessed in connection with mucosal healing (MH) and mucosal response (MR) defined per sMaRIA guidelines as a global sMaRIA < 5 and decrease in sMaRIA ≥ 50% respectively.
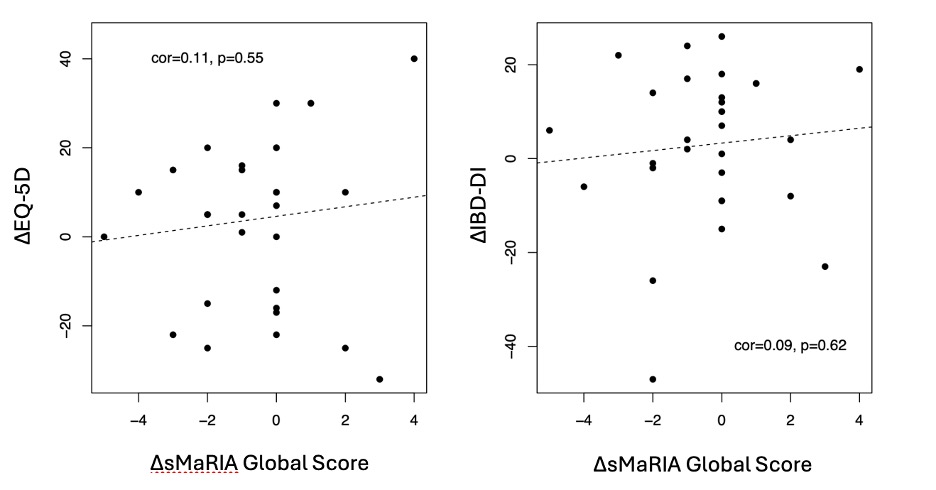
Results: At Week 0, mean IBD-DI, EQ-5D visual analogue scale, and sMaRIA values were -8.08, 75.80, and 1.87. At Week 52, mean IBD-DI, EQ-5D, and sMaRIA were -5.24, 77.90, and 1.49. IBD-DI and EQ-5D scores did not show significant association with global sMaRIA (p=0.06, p=0.42). Neither change in IBD-DI nor EQ-5D were associated with progression of sMaRIA scores from Week 0 to Week 52 by multivariate regression models (p=0.79, p=0.95) adjusting for gender, BMI, race, and Montreal disease classification. Change in IBD-DI and EQ-5D scores was not associated with development of MH (p=0.94, p=0.71) or MR (p=0.66, p=0.45) by week 52.
Discussion: In our analysis, there was no significant connection between IBD-DI and/or EQ-5D questionnaire scores and inflammation or healing on MRE. This highlights a potential need for improved patient-reported wellness surveys to reflect true disease activity. Further study is warranted to determine possible utility of IBD-DI and EQ-5D in CD management.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Brett D. Riederman, MD1, Richard Tsai, MD2, Chongliang Luo, PhD2, David Ballard, MD2, Parakkal Deepak, MBBS, MS3. P2582 - Examining the Relationship Between Transmural Response on MRE and Subjective Wellness Assessments in Small Bowel Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, MO; 2Washington University School of Medicine in St. Louis, St. Louis, MO; 3Washington University in St. Louis, St. Louis, MO
Introduction: In Crohn’s disease (CD), treatment goals have advanced over time with an objective of deep remission: absence of symptoms along with mucosal healing (MH) observed on ileocolonoscopy. In patients with small bowel CD, magnetic resonance enterography (MRE) has been used in place of ileocolonoscopy with a goal of assessing transmural response (TR). While TR may be a useful target in evaluating inflammation, it is not known whether this correlates with improvement in disease symptoms. We sought to determine if degree of inflammation on MRE is associated with subjective wellness measures.
Methods: We analyzed a cohort of 83 patients ages 18-80 with small bowel CD seen in Washington University IBD clinics. Initial visits took place from 2018 to 2021 with Week 0 Inflammatory Bowel Disease Disability Index (IBD-DI) and EQ-5D questionnaires completed at that time. This was repeated for those with visits at Week 52. Subjects also had a week 0 MRE which was completed within one year prior to initial clinic visit with week 52 MRE done within one month of week 52 visit. Each MRE was assessed by a specialized GI radiologist and scored using the simplified Magnetic Resonance Index of Activity (sMaRIA). Difference between Week 0 and 52 questionnaire scores was compared directly with associated sMaRIA values. Change in questionnaire scores was also assessed in connection with mucosal healing (MH) and mucosal response (MR) defined per sMaRIA guidelines as a global sMaRIA < 5 and decrease in sMaRIA ≥ 50% respectively.
Results: At Week 0, mean IBD-DI, EQ-5D visual analogue scale, and sMaRIA values were -8.08, 75.80, and 1.87. At Week 52, mean IBD-DI, EQ-5D, and sMaRIA were -5.24, 77.90, and 1.49. IBD-DI and EQ-5D scores did not show significant association with global sMaRIA (p=0.06, p=0.42). Neither change in IBD-DI nor EQ-5D were associated with progression of sMaRIA scores from Week 0 to Week 52 by multivariate regression models (p=0.79, p=0.95) adjusting for gender, BMI, race, and Montreal disease classification. Change in IBD-DI and EQ-5D scores was not associated with development of MH (p=0.94, p=0.71) or MR (p=0.66, p=0.45) by week 52.
Discussion: In our analysis, there was no significant connection between IBD-DI and/or EQ-5D questionnaire scores and inflammation or healing on MRE. This highlights a potential need for improved patient-reported wellness surveys to reflect true disease activity. Further study is warranted to determine possible utility of IBD-DI and EQ-5D in CD management.
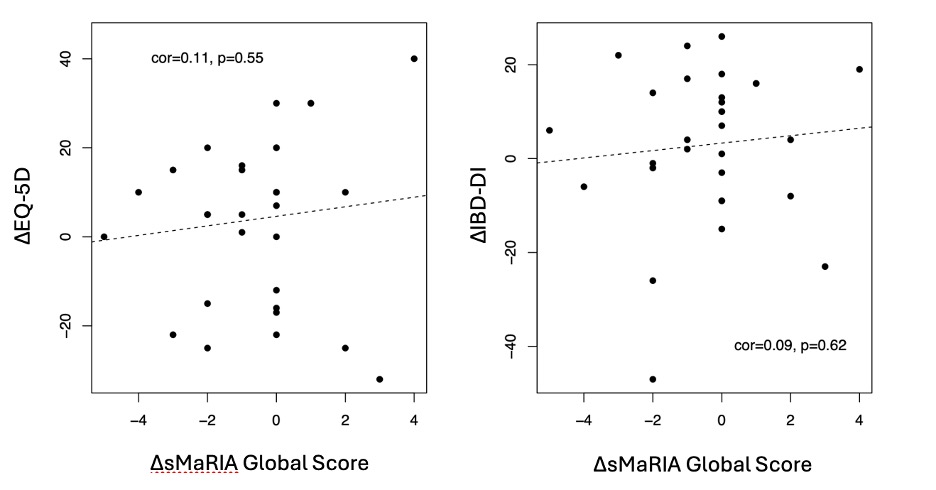
Figure: Figure 1. Questionnaire scores and sMaRIA as a function of time
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Brett Riederman indicated no relevant financial relationships.
Richard Tsai indicated no relevant financial relationships.
Chongliang Luo indicated no relevant financial relationships.
David Ballard: Merck – Consultant.
Parakkal Deepak: AbbVie – Consultant, Grant/Research Support. Alimentiv – Grant/Research Support. Arena Pharmaceuticals – Grant/Research Support. Boehringer Ingelheim – Grant/Research Support. Bristol Myers Squibb-Celgene – Advisory Committee/Board Member, Grant/Research Support. CorEvitas LLC – Consultant. Janssen – Grant/Research Support. Pfizer – Grant/Research Support. Prometheus Biosciences – Grant/Research Support. Roche/Genentech – Advisory Committee/Board Member. Scipher Medicine – Grant/Research Support. Takeda – Grant/Research Support.
Brett D. Riederman, MD1, Richard Tsai, MD2, Chongliang Luo, PhD2, David Ballard, MD2, Parakkal Deepak, MBBS, MS3. P2582 - Examining the Relationship Between Transmural Response on MRE and Subjective Wellness Assessments in Small Bowel Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
