Monday Poster Session
Category: GI Bleeding
P2513 - Gastrointestinal Stromal Tumor Presenting as a Life-Threatening Lower Gastrointestinal Bleed
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- DJ
Divij K. Jha, MD
Sparrow Hospital, Michigan State University
Lansing, MI
Presenting Author(s)
Divij K. Jha, MD1, Amey Joshi, MD1, Harith Ghnaima, MD2, Richa Tikaria, MD3
1Sparrow Hospital, Michigan State University, Lansing, MI; 2Sparrow Hospital, Michigan State University, East Lansing, MI; 3Michigan State University College of Human Medicine, Lansing, MI
Introduction: Gastrointestinal stromal tumors (GISTs) often present with nonspecific clinical manifestations and may be found incidentally on endoscopy or surgery. The most frequently reported symptoms include gastrointestinal bleeding, abdominal pain, weight loss, and palpable abdominal mass. Herein, we present a rare case of an ileal GIST that presented with massive lower gastrointestinal bleeding requiring multiple blood transfusions.
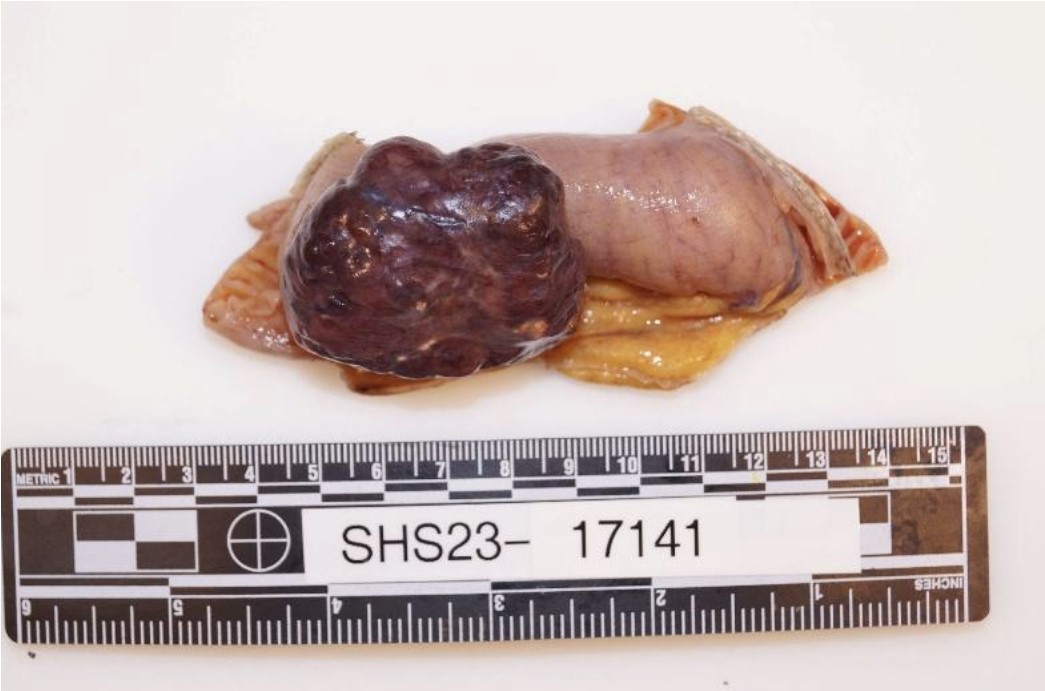
Case Description/Methods: A 71-year-old female with a history of diverticulosis presented with multiple episodes of bright red bowel movements and diffuse abdominal pain for 2 days. She was noted to be anemic (Hb 5.9 g/dl), and CT angiography revealed a brisk upper gastrointestinal bleed in the ileal region. Initial EGD failed to reveal signs of active bleeding from the duodenum, so an emergent selective mesenteric angiography with embolization to the distal branches of the dominant ileal artery was done. Due to persisting symptoms, a repeat CTA of the abdomen revealed a hyper-enhancing exophytic 4.7 x 3 x 4.1 cm lesion in the proximal ileal region. The patient underwent laparoscopic excision of the mass with small bowel resection and anastomosis that led to the resolution of symptoms. The pathology sample confirmed low-grade GIST with negative margins and positive immunohistochemical staining with CD117 and DOG1.
Discussion: GISTs are very rare neoplasms found in the stomach and small intestine. When symptomatic, GISTs can present with nonspecific symptoms such as dysphagia, abdominal pain, and bloating. Depending on their location, they may also cause upper or lower gastrointestinal bleeding, colonic perforation, pain, or obstruction. Endoscopy may be able to detect intraluminal growth in only 60% of cases, and EUS-FNA may improve detection rates. CT imaging remains the ideal tool for detecting GISTs > 2cm, as seen in the present case. Although GIST morphology is varied, immunohistochemical staining usually establishes the diagnosis. Surgery remains the mainstay for the treatment of symptomatic GISTs, especially those presenting with massive GI hemorrhage, as seen in the present case. Through the present case, we highlight the crucial role of CT imaging in the setting of normal upper GI endoscopy and the resolution of life-threatening hemorrhage with prompt surgical intervention.
Disclosures:
Divij K. Jha, MD1, Amey Joshi, MD1, Harith Ghnaima, MD2, Richa Tikaria, MD3. P2513 - Gastrointestinal Stromal Tumor Presenting as a Life-Threatening Lower Gastrointestinal Bleed, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Sparrow Hospital, Michigan State University, Lansing, MI; 2Sparrow Hospital, Michigan State University, East Lansing, MI; 3Michigan State University College of Human Medicine, Lansing, MI
Introduction: Gastrointestinal stromal tumors (GISTs) often present with nonspecific clinical manifestations and may be found incidentally on endoscopy or surgery. The most frequently reported symptoms include gastrointestinal bleeding, abdominal pain, weight loss, and palpable abdominal mass. Herein, we present a rare case of an ileal GIST that presented with massive lower gastrointestinal bleeding requiring multiple blood transfusions.
Case Description/Methods: A 71-year-old female with a history of diverticulosis presented with multiple episodes of bright red bowel movements and diffuse abdominal pain for 2 days. She was noted to be anemic (Hb 5.9 g/dl), and CT angiography revealed a brisk upper gastrointestinal bleed in the ileal region. Initial EGD failed to reveal signs of active bleeding from the duodenum, so an emergent selective mesenteric angiography with embolization to the distal branches of the dominant ileal artery was done. Due to persisting symptoms, a repeat CTA of the abdomen revealed a hyper-enhancing exophytic 4.7 x 3 x 4.1 cm lesion in the proximal ileal region. The patient underwent laparoscopic excision of the mass with small bowel resection and anastomosis that led to the resolution of symptoms. The pathology sample confirmed low-grade GIST with negative margins and positive immunohistochemical staining with CD117 and DOG1.
Discussion: GISTs are very rare neoplasms found in the stomach and small intestine. When symptomatic, GISTs can present with nonspecific symptoms such as dysphagia, abdominal pain, and bloating. Depending on their location, they may also cause upper or lower gastrointestinal bleeding, colonic perforation, pain, or obstruction. Endoscopy may be able to detect intraluminal growth in only 60% of cases, and EUS-FNA may improve detection rates. CT imaging remains the ideal tool for detecting GISTs > 2cm, as seen in the present case. Although GIST morphology is varied, immunohistochemical staining usually establishes the diagnosis. Surgery remains the mainstay for the treatment of symptomatic GISTs, especially those presenting with massive GI hemorrhage, as seen in the present case. Through the present case, we highlight the crucial role of CT imaging in the setting of normal upper GI endoscopy and the resolution of life-threatening hemorrhage with prompt surgical intervention.
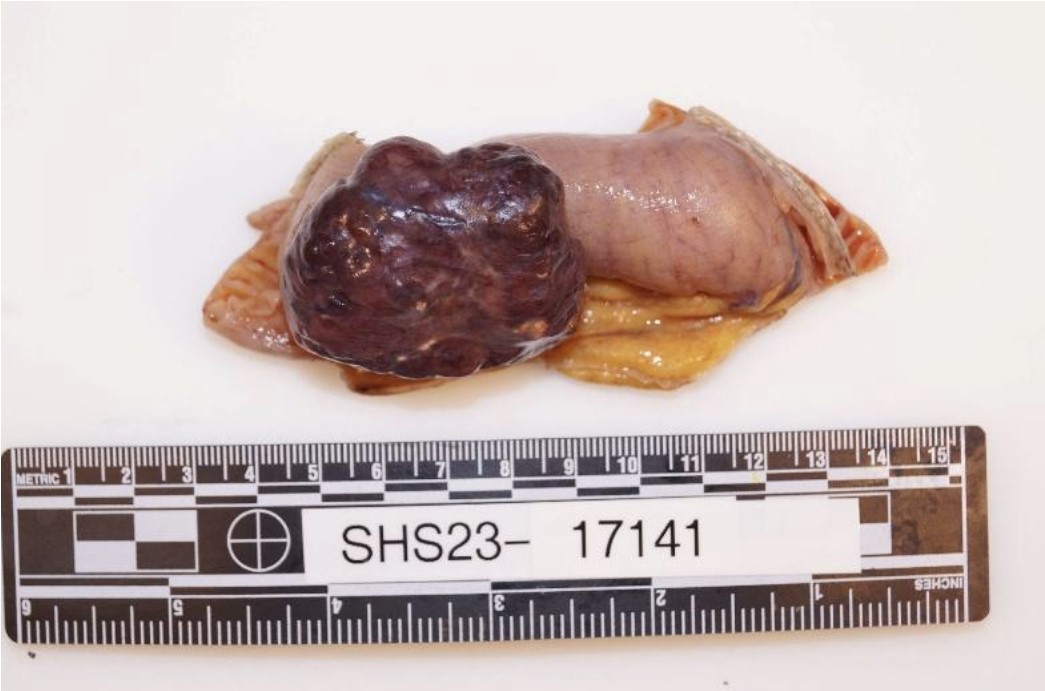
Figure: Resected small-bowel gastrointestinal stromal tumor (GIST)
Disclosures:
Divij Jha indicated no relevant financial relationships.
Amey Joshi indicated no relevant financial relationships.
Harith Ghnaima indicated no relevant financial relationships.
Richa Tikaria indicated no relevant financial relationships.
Divij K. Jha, MD1, Amey Joshi, MD1, Harith Ghnaima, MD2, Richa Tikaria, MD3. P2513 - Gastrointestinal Stromal Tumor Presenting as a Life-Threatening Lower Gastrointestinal Bleed, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
