Monday Poster Session
Category: GI Bleeding
P2517 - Rare Vascular Complication of Pancreatitis: Hemorrhagic Pseudocyst Caused by Gastroduodenal Artery Pseudoaneurysm Despite Prior Embolization
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- JS
Judy Sheffeh, MD
Ascension Macomb-Oakland Hospital
Warren, MI
Presenting Author(s)
Benjamin Cavanaugh, MS, Judy Sheffeh, MD, Sunpreet Singh, DO, Mohammad Ali Sheffeh, MD, Nafea Majed Zayouna, MD
Ascension Macomb-Oakland Hospital, Warren, MI
Introduction: Acute and chronic pancreatitis can lead to pancreatic pseudocyst formation, occurring in around 40% of those with alcohol-induced chronic pancreatitis. Pancreatic pseudoaneurysm arises from artery erosion into the pseudocyst. Hemorrhagic pancreatic pseudocysts due to pseudoaneurysm occur with an incidence rate of 6% to 17%, carrying a mortality rate of 40%. We are reporting a rare case of gastroduodenal artery (GDA) pseudoaneurysm complicated by hemorrhage despite a prior history of coil embolization. GDA aneurysms represent only 1.5% of documented visceral artery aneurysms, the majority of which are pseudoaneurysms
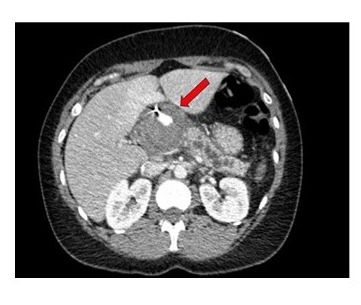
Case Description/Methods: A 39-year-old Female with alcohol-induced chronic pancreatitis, and a history of large GDA pseudoaneurysm with previous selective coil embolization, presented with 3 days of epigastric pain, nausea, vomiting, and lightheadedness. Exquisite tenderness in the epigastric area noted on exam. Initial labs revealed a critical Hemoglobin of 4.1. The Patient received 2 units of packed red blood cells. Computed tomography of the abdomen and pelvis showed a heterogeneous mass in the region of the pancreatic head/uncinate process that enlarged in the interval and measured 5.6 x 4.3 x 4.8 cm. A 1.7 cm focus of extravasated contrast was seen within the mass which possibly represented a pseudocyst with active bleeding (Figure 1). The interventional radiologist performed a mesenteric angiography and confirmed the presence of GDA pseudoaneurysm with hemorrhage. Coil embolization of the pseudoaneurysm was successful. The patient was transferred to the ICU for further monitoring and eventually was discharged home.
Discussion: Pancreatic pseudoaneurysms are rare, and predominantly caused by pancreatitis. Studies report that the most common location of pancreatic pseudoaneurysm is the splenic artery, followed by GDA, pancreaticoduodenal, left gastric, and common hepatic arteries. Gastrointestinal bleeding is the most common presenting symptom of GDA pseudoaneurysm (52%), followed by abdominal pain (46%). Diagnosing pseudoaneurysm becomes more challenging when abdominal pain is the sole symptom, as it may be attributed to various causes. There is still an increased risk of recurrence after embolization of pseudoaneurysm as seen in our patient, the mortality rate remains elevated at 16% after embolization. For the aforementioned reasons, it is paramount to maintain a high suspicion of the diagnosis in patients with pancreatitis to ensure prompt and appropriate treatment.
Disclosures:
Benjamin Cavanaugh, MS, Judy Sheffeh, MD, Sunpreet Singh, DO, Mohammad Ali Sheffeh, MD, Nafea Majed Zayouna, MD. P2517 - Rare Vascular Complication of Pancreatitis: Hemorrhagic Pseudocyst Caused by Gastroduodenal Artery Pseudoaneurysm Despite Prior Embolization, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Ascension Macomb-Oakland Hospital, Warren, MI
Introduction: Acute and chronic pancreatitis can lead to pancreatic pseudocyst formation, occurring in around 40% of those with alcohol-induced chronic pancreatitis. Pancreatic pseudoaneurysm arises from artery erosion into the pseudocyst. Hemorrhagic pancreatic pseudocysts due to pseudoaneurysm occur with an incidence rate of 6% to 17%, carrying a mortality rate of 40%. We are reporting a rare case of gastroduodenal artery (GDA) pseudoaneurysm complicated by hemorrhage despite a prior history of coil embolization. GDA aneurysms represent only 1.5% of documented visceral artery aneurysms, the majority of which are pseudoaneurysms
Case Description/Methods: A 39-year-old Female with alcohol-induced chronic pancreatitis, and a history of large GDA pseudoaneurysm with previous selective coil embolization, presented with 3 days of epigastric pain, nausea, vomiting, and lightheadedness. Exquisite tenderness in the epigastric area noted on exam. Initial labs revealed a critical Hemoglobin of 4.1. The Patient received 2 units of packed red blood cells. Computed tomography of the abdomen and pelvis showed a heterogeneous mass in the region of the pancreatic head/uncinate process that enlarged in the interval and measured 5.6 x 4.3 x 4.8 cm. A 1.7 cm focus of extravasated contrast was seen within the mass which possibly represented a pseudocyst with active bleeding (Figure 1). The interventional radiologist performed a mesenteric angiography and confirmed the presence of GDA pseudoaneurysm with hemorrhage. Coil embolization of the pseudoaneurysm was successful. The patient was transferred to the ICU for further monitoring and eventually was discharged home.
Discussion: Pancreatic pseudoaneurysms are rare, and predominantly caused by pancreatitis. Studies report that the most common location of pancreatic pseudoaneurysm is the splenic artery, followed by GDA, pancreaticoduodenal, left gastric, and common hepatic arteries. Gastrointestinal bleeding is the most common presenting symptom of GDA pseudoaneurysm (52%), followed by abdominal pain (46%). Diagnosing pseudoaneurysm becomes more challenging when abdominal pain is the sole symptom, as it may be attributed to various causes. There is still an increased risk of recurrence after embolization of pseudoaneurysm as seen in our patient, the mortality rate remains elevated at 16% after embolization. For the aforementioned reasons, it is paramount to maintain a high suspicion of the diagnosis in patients with pancreatitis to ensure prompt and appropriate treatment.
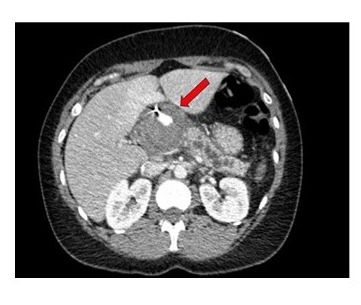
Figure: Figure 1: CT Abdomen And Pelvis Showing Changes Suggestive of Acute on Chronic Pancreatitis, Pancreatic Pseudocyst With Possible Hemorrhage.
Disclosures:
Benjamin Cavanaugh indicated no relevant financial relationships.
Judy Sheffeh indicated no relevant financial relationships.
Sunpreet Singh indicated no relevant financial relationships.
Mohammad Ali Sheffeh indicated no relevant financial relationships.
Nafea Majed Zayouna indicated no relevant financial relationships.
Benjamin Cavanaugh, MS, Judy Sheffeh, MD, Sunpreet Singh, DO, Mohammad Ali Sheffeh, MD, Nafea Majed Zayouna, MD. P2517 - Rare Vascular Complication of Pancreatitis: Hemorrhagic Pseudocyst Caused by Gastroduodenal Artery Pseudoaneurysm Despite Prior Embolization, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
