Monday Poster Session
Category: GI Bleeding
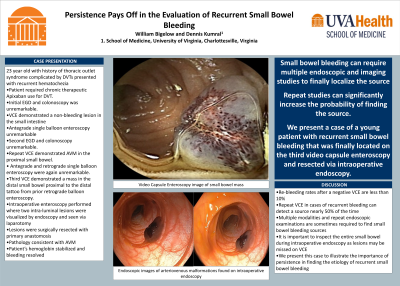
P2519 - Persistence Pays Off in the Evaluation of Recurrent Small Bowel Bleeding
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- WB
William Bigelow, MD
University of Virginia
Charlottesville, VA
Presenting Author(s)
William Bigelow, MD, Dennis Kumral, MD
University of Virginia, Charlottesville, VA
Introduction: Small bowel gastrointestinal bleeding can be difficult to evaluate and manage. The majority of these cases are due to arteriovenous malformations (AVM) of the small intestine in elderly patients. We present a case of a young patient requiring anticoagulation with recurrent gastrointestinal bleeding requiring multiple endoscopic evaluations and ultimately intraoperative enteroscopy for definitive management.
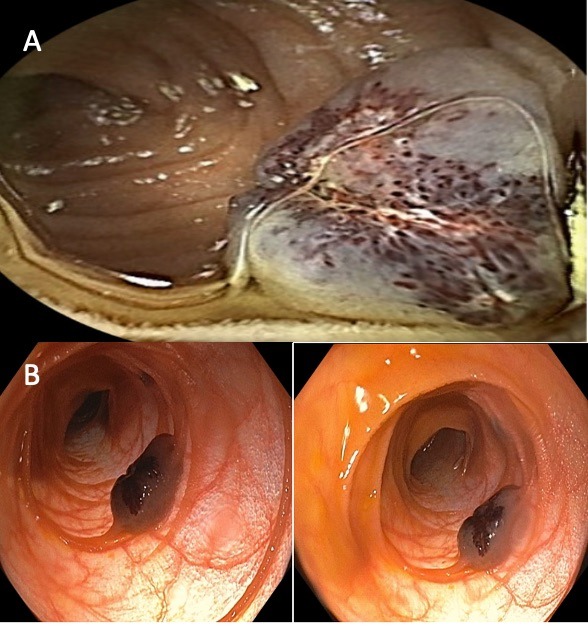
Case Description/Methods: A 23-year-old female with history of thoracic outlet syndrome complicated by upper extremity DVTs for which she was on therapeutic Apixaban presented with recurrent hematochezia. The patient had initially presented with iron deficiency anemia and unremarkable esophagogastroduodenoscopy (EGD) and colonoscopy. Video capsule enteroscopy (VCE) demonstrated a non-bleeding lesion in the small intestine though subsequent antegrade single balloon enteroscopy was unremarkable. She represented one year later with overt GI bleeding. A repeat EGD and colonoscopy were again normal. VCE demonstrated an AVM in the small intestine with active bleeding. She then underwent antegrade and retrograde single balloon enteroscopy that were both unremarkable. Her overt GI bleeding resolved and hemoglobin stabilized. She then presented for a third admission with overt GI bleeding. Repeat VCE demonstrated a mass in the distal small bowel that appeared to be a lymphangiectasia (Figure 1A) proximal to the distal tattoo from prior retrograde balloon enteroscopy. She underwent intraoperative enteroscopy where two lesions were removed. The lesions were visualized endoscopically as well as externally during the operation (Figure 1B). Pathology for both lesions was consistent with AVM and not lymphangiectasia. After the operation, the patient's hemoglobin stabilized and her hematochezia resolved.
Discussion: Multiple modalities and repeated endoscopic evaluations are sometimes required to determine etiologies of small bowel bleeding. While re-bleeding rates after a negative VCE are less than 10%, a repeat VCE in recurrent bleeding will detect a source in nearly 50% of cases. Our patient ultimately required three VCE prior to discovering an identifiable source. While only one lesion was noted on VCE, two lesions were found intraoperatively. Intraoperative enteroscopy allows for evaluation of the entire small bowel and when applied in the right case can isolate the bleeding source even in the most difficult cases of small bowel bleeding.
Disclosures:
William Bigelow, MD, Dennis Kumral, MD. P2519 - Persistence Pays Off in the Evaluation of Recurrent Small Bowel Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Virginia, Charlottesville, VA
Introduction: Small bowel gastrointestinal bleeding can be difficult to evaluate and manage. The majority of these cases are due to arteriovenous malformations (AVM) of the small intestine in elderly patients. We present a case of a young patient requiring anticoagulation with recurrent gastrointestinal bleeding requiring multiple endoscopic evaluations and ultimately intraoperative enteroscopy for definitive management.
Case Description/Methods: A 23-year-old female with history of thoracic outlet syndrome complicated by upper extremity DVTs for which she was on therapeutic Apixaban presented with recurrent hematochezia. The patient had initially presented with iron deficiency anemia and unremarkable esophagogastroduodenoscopy (EGD) and colonoscopy. Video capsule enteroscopy (VCE) demonstrated a non-bleeding lesion in the small intestine though subsequent antegrade single balloon enteroscopy was unremarkable. She represented one year later with overt GI bleeding. A repeat EGD and colonoscopy were again normal. VCE demonstrated an AVM in the small intestine with active bleeding. She then underwent antegrade and retrograde single balloon enteroscopy that were both unremarkable. Her overt GI bleeding resolved and hemoglobin stabilized. She then presented for a third admission with overt GI bleeding. Repeat VCE demonstrated a mass in the distal small bowel that appeared to be a lymphangiectasia (Figure 1A) proximal to the distal tattoo from prior retrograde balloon enteroscopy. She underwent intraoperative enteroscopy where two lesions were removed. The lesions were visualized endoscopically as well as externally during the operation (Figure 1B). Pathology for both lesions was consistent with AVM and not lymphangiectasia. After the operation, the patient's hemoglobin stabilized and her hematochezia resolved.
Discussion: Multiple modalities and repeated endoscopic evaluations are sometimes required to determine etiologies of small bowel bleeding. While re-bleeding rates after a negative VCE are less than 10%, a repeat VCE in recurrent bleeding will detect a source in nearly 50% of cases. Our patient ultimately required three VCE prior to discovering an identifiable source. While only one lesion was noted on VCE, two lesions were found intraoperatively. Intraoperative enteroscopy allows for evaluation of the entire small bowel and when applied in the right case can isolate the bleeding source even in the most difficult cases of small bowel bleeding.
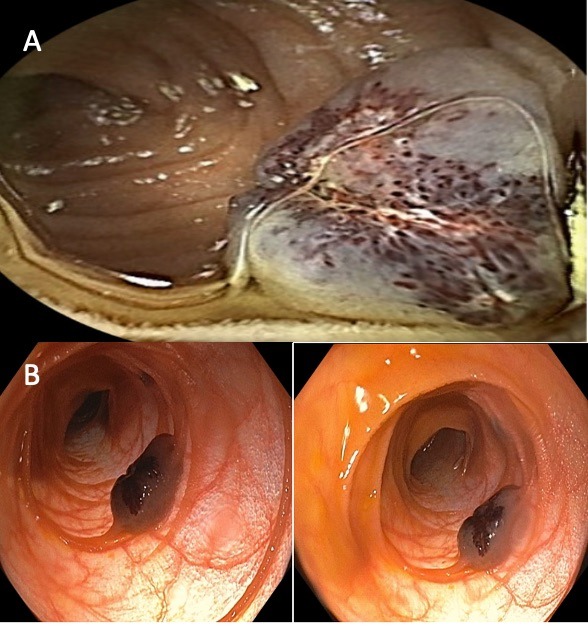
Figure: Figure 1. A) Video capsule enteroscopy image of small intestine lesion initially believed to be lympangiectasia though later confirmed to be arteriovenous malformation. B) Endoscopic images of arteriovenous malformation
Disclosures:
William Bigelow indicated no relevant financial relationships.
Dennis Kumral indicated no relevant financial relationships.
William Bigelow, MD, Dennis Kumral, MD. P2519 - Persistence Pays Off in the Evaluation of Recurrent Small Bowel Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
