Monday Poster Session
Category: GI Bleeding
P2521 - A Rare Case of Gastrointestinal Bleeding Secondary to Gastric Mucormycosis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Chimsom Orakwue, MD
New York-Presbyterian / Weill Cornell Medical Center
New York, NY
Presenting Author(s)
Chimsom Orakwue, MD1, Malik Mushannen, MD2, Aiya Aboubakr, MD1, Eliza Cricco-Lizza, MD1, Carl V. Crawford, MD1
1New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian / Brooklyn Methodist Hospital, Brooklyn, NY
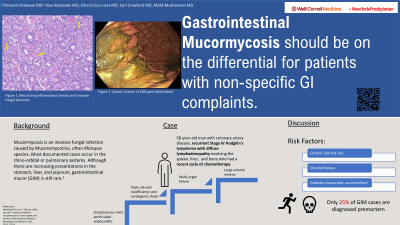
Introduction: Mucormycosis is an invasive fungal infection caused by Mucoromycotina, often Rhizopus species. Most documented cases occur in the rhino-orbital or pulmonary systems. Although there are increasing presentations in the stomach, liver, and jejunum, gastrointestinal mucor (GIM) is still rare1. This case featured a presentation of gastrointestinal bleeding (GIB) secondary to GIM.
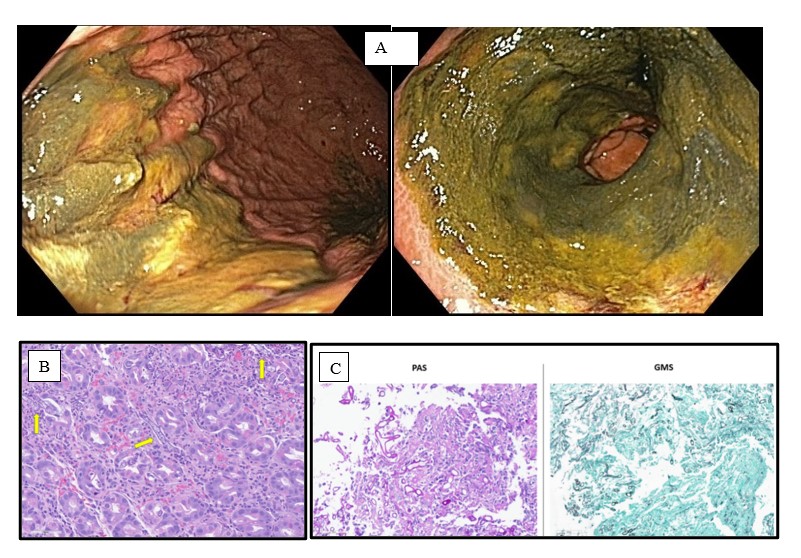
Case Description/Methods: A 58-year-old man with coronary artery disease, recurrent Stage IV Hodgkin's lymphoma with diffuse lymphadenopathy (spleen, liver, bone) and recent chemotherapy (brentuximab vedotin plus doxorubicin, vinblastine, dacarbazine), was admitted for management of acute Streptococcus mitis aortic valve endocarditis complicated by severe triple valvular insufficiency and cardiogenic shock for which he had serial valve replacements. His course was complicated by multiorgan failure (respiratory requiring tracheostomy, renal requiring dialysis),and large-volume melena for which GI was consulted. Endoscopy showed diffuse, confluent, highly friable mucosal inflammation with ulceration and green exudate in the antrum and greater stomach curvature (Fig1a). Biopsies showed necrotizing inflammatory lesions (Fig 1b). PAS stain confirmed candida and Rhizomucor(Fig 1c). He was treated with isavuconazole and switched to amphotericin for increased efficacy. Repeat endoscopy was performed due to persistent anemia requiring multiple transfusions, which revealed mucosal healing without active bleeding.
Discussion: We present a case of GIM causing significant GIB in a patient with end-stage Hodgkin’s lymphoma. In literature, only 25% of GIM cases are diagnosed premortem due to its rapid, fatal progression1 and nonspecific symptoms that make early diagnosis difficult. Most cases go unnoticed unless incidentally diagnosed on endoscopy, however, GIM has potential to cause necrotizing inflammation. Risk factors for infection include chemotherapy-related immunosuppression, chronic steroid use, and poorly controlled diabetes. It is important to consider GIM on the differential for patients with such risk factors presenting with nonspecific GI complaints and to pursue biopsy in those with GIB. Patients may benefit from early antifungal use, however typically mucosal injury is so severe at time of diagnosis that hemostasis is challenging and often unsuccessful.1
1. Martinello M, et al. “We are what we eat!” Invasive intestinal mucormycosis: A case report and review of the literature, Medical Mycology Case Reports; 1(1), 2012: 52-55.
Disclosures:
Chimsom Orakwue, MD1, Malik Mushannen, MD2, Aiya Aboubakr, MD1, Eliza Cricco-Lizza, MD1, Carl V. Crawford, MD1. P2521 - A Rare Case of Gastrointestinal Bleeding Secondary to Gastric Mucormycosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian / Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Mucormycosis is an invasive fungal infection caused by Mucoromycotina, often Rhizopus species. Most documented cases occur in the rhino-orbital or pulmonary systems. Although there are increasing presentations in the stomach, liver, and jejunum, gastrointestinal mucor (GIM) is still rare1. This case featured a presentation of gastrointestinal bleeding (GIB) secondary to GIM.
Case Description/Methods: A 58-year-old man with coronary artery disease, recurrent Stage IV Hodgkin's lymphoma with diffuse lymphadenopathy (spleen, liver, bone) and recent chemotherapy (brentuximab vedotin plus doxorubicin, vinblastine, dacarbazine), was admitted for management of acute Streptococcus mitis aortic valve endocarditis complicated by severe triple valvular insufficiency and cardiogenic shock for which he had serial valve replacements. His course was complicated by multiorgan failure (respiratory requiring tracheostomy, renal requiring dialysis),and large-volume melena for which GI was consulted. Endoscopy showed diffuse, confluent, highly friable mucosal inflammation with ulceration and green exudate in the antrum and greater stomach curvature (Fig1a). Biopsies showed necrotizing inflammatory lesions (Fig 1b). PAS stain confirmed candida and Rhizomucor(Fig 1c). He was treated with isavuconazole and switched to amphotericin for increased efficacy. Repeat endoscopy was performed due to persistent anemia requiring multiple transfusions, which revealed mucosal healing without active bleeding.
Discussion: We present a case of GIM causing significant GIB in a patient with end-stage Hodgkin’s lymphoma. In literature, only 25% of GIM cases are diagnosed premortem due to its rapid, fatal progression1 and nonspecific symptoms that make early diagnosis difficult. Most cases go unnoticed unless incidentally diagnosed on endoscopy, however, GIM has potential to cause necrotizing inflammation. Risk factors for infection include chemotherapy-related immunosuppression, chronic steroid use, and poorly controlled diabetes. It is important to consider GIM on the differential for patients with such risk factors presenting with nonspecific GI complaints and to pursue biopsy in those with GIB. Patients may benefit from early antifungal use, however typically mucosal injury is so severe at time of diagnosis that hemostasis is challenging and often unsuccessful.1
1. Martinello M, et al. “We are what we eat!” Invasive intestinal mucormycosis: A case report and review of the literature, Medical Mycology Case Reports; 1(1), 2012: 52-55.
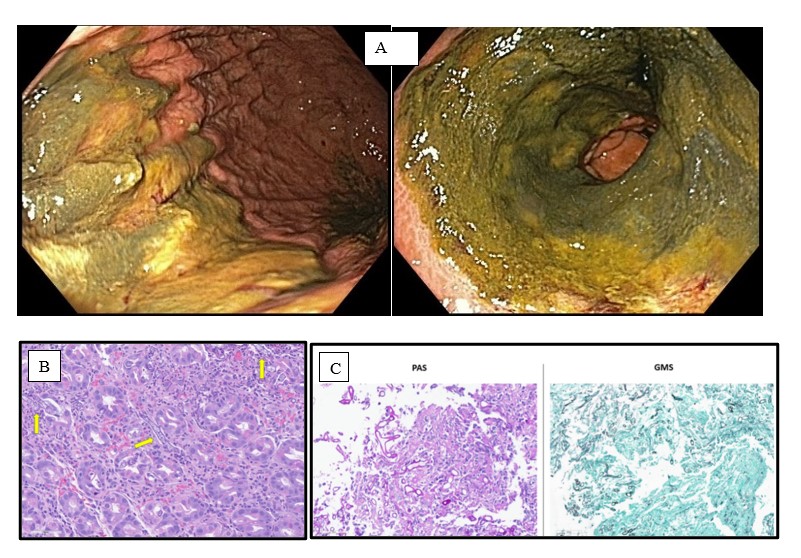
Figure: Figure 1A: Gastric Antrum;
Figure 1B: Necrotizing inflammatory lesions and invasive fungal elements;
Figure 1C: Non-pigmented (hyaline), pauciseptate ribbonlike hyphae with right-angle branching consistent with Mucorales
Figure 1B: Necrotizing inflammatory lesions and invasive fungal elements;
Figure 1C: Non-pigmented (hyaline), pauciseptate ribbonlike hyphae with right-angle branching consistent with Mucorales
Disclosures:
Chimsom Orakwue indicated no relevant financial relationships.
Malik Mushannen indicated no relevant financial relationships.
Aiya Aboubakr indicated no relevant financial relationships.
Eliza Cricco-Lizza indicated no relevant financial relationships.
Carl Crawford: Ferring – Grant/Research Support. Nestle – Speakers Bureau. Phathom – Speakers Bureau. Seres – Speakers Bureau. Vedanta – Grant/Research Support.
Chimsom Orakwue, MD1, Malik Mushannen, MD2, Aiya Aboubakr, MD1, Eliza Cricco-Lizza, MD1, Carl V. Crawford, MD1. P2521 - A Rare Case of Gastrointestinal Bleeding Secondary to Gastric Mucormycosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
