Monday Poster Session
Category: GI Bleeding
P2524 - Duodenal Varices as a Rare Etiology of Upper GI Bleeding in a Patient With Roux-en-Y Gastric Bypass Anatomy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Ruona Ebiai, MD
Ochsner Health Clinic Foundation
New Orleans, LA
Presenting Author(s)
Ruona Ebiai, MD, Jasmine McNair, MD, Jordan Boudreaux, MD, Ravi Jariwala, MD, Kelli Morgan, MD
Ochsner Health Clinic Foundation, New Orleans, LA
Introduction: Duodenal Varices are a very rare cause of upper gastrointestinal hemorrhage and account for only 1-5% of all variceal bleeding. These varices carry a significant mortality risk of up to 40%. Roux-en-Y gastric bypass anatomy can further add to the difficulty of localizing and managing duodenal varices. Here we report a case of a 44-year-old woman with prior Roux-en-Y gastric bypass who required repeated endoscopic evaluation to identify bleeding duodenal varices.
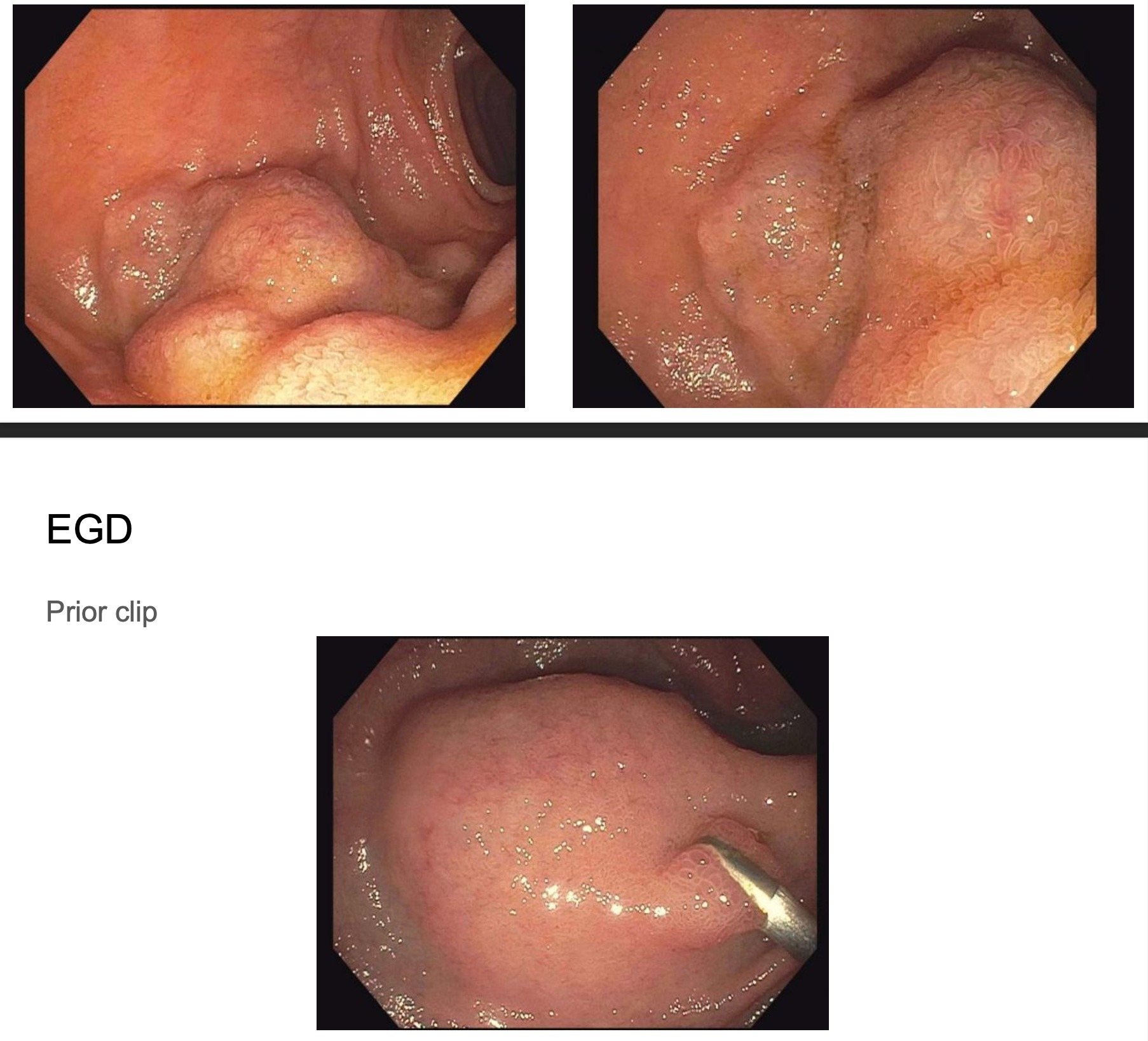
Case Description/Methods: A 44-year-old woman with a medical history of decompensated alcoholic cirrhosis and Roux-en-Y gastric bypass surgery (2010) presented to the hospital for cramping epigastric abdominal pain and melena. Four months prior, she was evaluated for a similar presentation. Small bowel enteroscopy performed at that time revealed gastrojejunal anastomosis characterized by healthy appearing mucosa but fresh blood in the afferent limb. A marking clip was placed near the bleeding which was around the ampulla. No varices were identified. She improved over that hospital stay and was able to be discharged home. Physical examination on this admission revealed tachycardia and abdominal tenderness in the epigastric and left lower quadrant. Initial labs showed hemoglobin 6.0 g/dL and platelet count 315,000 /mm3. She received 1 unit of packed-red blood cells. Small bowel enteroscopy was performed the next day which demonstrated two large duodenal varices in two discrete areas of the afferent limb. Hemoclip was still present near one of the duodenal varices. Given these new findings, hepatology was consulted to assess if the patient would be a good candidate for a transjugular intrahepatic portosystemic shunt (TIPS) procedure. No contraindications were noted. Interventional Radiology was consulted for TIPS procedure with embolization of duodenal varices which was successfully done two days later. Hepatic venous pressure gradient (HVPG) was reduced from 18 to 4. No further bleeding was reported and the patient was discharged home two days later. At her post-discharge PCP visit, she reported no further bleeding.
Discussion: Recognition of duodenal varices as the source of hemorrhage can be challenging and might take up to multiple repeated endoscopic evaluations before the definitive diagnosis can be made. Given its life-threatening nature, prompt diagnosis and early intervention is imperative.
Disclosures:
Ruona Ebiai, MD, Jasmine McNair, MD, Jordan Boudreaux, MD, Ravi Jariwala, MD, Kelli Morgan, MD. P2524 - Duodenal Varices as a Rare Etiology of Upper GI Bleeding in a Patient With Roux-en-Y Gastric Bypass Anatomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Ochsner Health Clinic Foundation, New Orleans, LA
Introduction: Duodenal Varices are a very rare cause of upper gastrointestinal hemorrhage and account for only 1-5% of all variceal bleeding. These varices carry a significant mortality risk of up to 40%. Roux-en-Y gastric bypass anatomy can further add to the difficulty of localizing and managing duodenal varices. Here we report a case of a 44-year-old woman with prior Roux-en-Y gastric bypass who required repeated endoscopic evaluation to identify bleeding duodenal varices.
Case Description/Methods: A 44-year-old woman with a medical history of decompensated alcoholic cirrhosis and Roux-en-Y gastric bypass surgery (2010) presented to the hospital for cramping epigastric abdominal pain and melena. Four months prior, she was evaluated for a similar presentation. Small bowel enteroscopy performed at that time revealed gastrojejunal anastomosis characterized by healthy appearing mucosa but fresh blood in the afferent limb. A marking clip was placed near the bleeding which was around the ampulla. No varices were identified. She improved over that hospital stay and was able to be discharged home. Physical examination on this admission revealed tachycardia and abdominal tenderness in the epigastric and left lower quadrant. Initial labs showed hemoglobin 6.0 g/dL and platelet count 315,000 /mm3. She received 1 unit of packed-red blood cells. Small bowel enteroscopy was performed the next day which demonstrated two large duodenal varices in two discrete areas of the afferent limb. Hemoclip was still present near one of the duodenal varices. Given these new findings, hepatology was consulted to assess if the patient would be a good candidate for a transjugular intrahepatic portosystemic shunt (TIPS) procedure. No contraindications were noted. Interventional Radiology was consulted for TIPS procedure with embolization of duodenal varices which was successfully done two days later. Hepatic venous pressure gradient (HVPG) was reduced from 18 to 4. No further bleeding was reported and the patient was discharged home two days later. At her post-discharge PCP visit, she reported no further bleeding.
Discussion: Recognition of duodenal varices as the source of hemorrhage can be challenging and might take up to multiple repeated endoscopic evaluations before the definitive diagnosis can be made. Given its life-threatening nature, prompt diagnosis and early intervention is imperative.
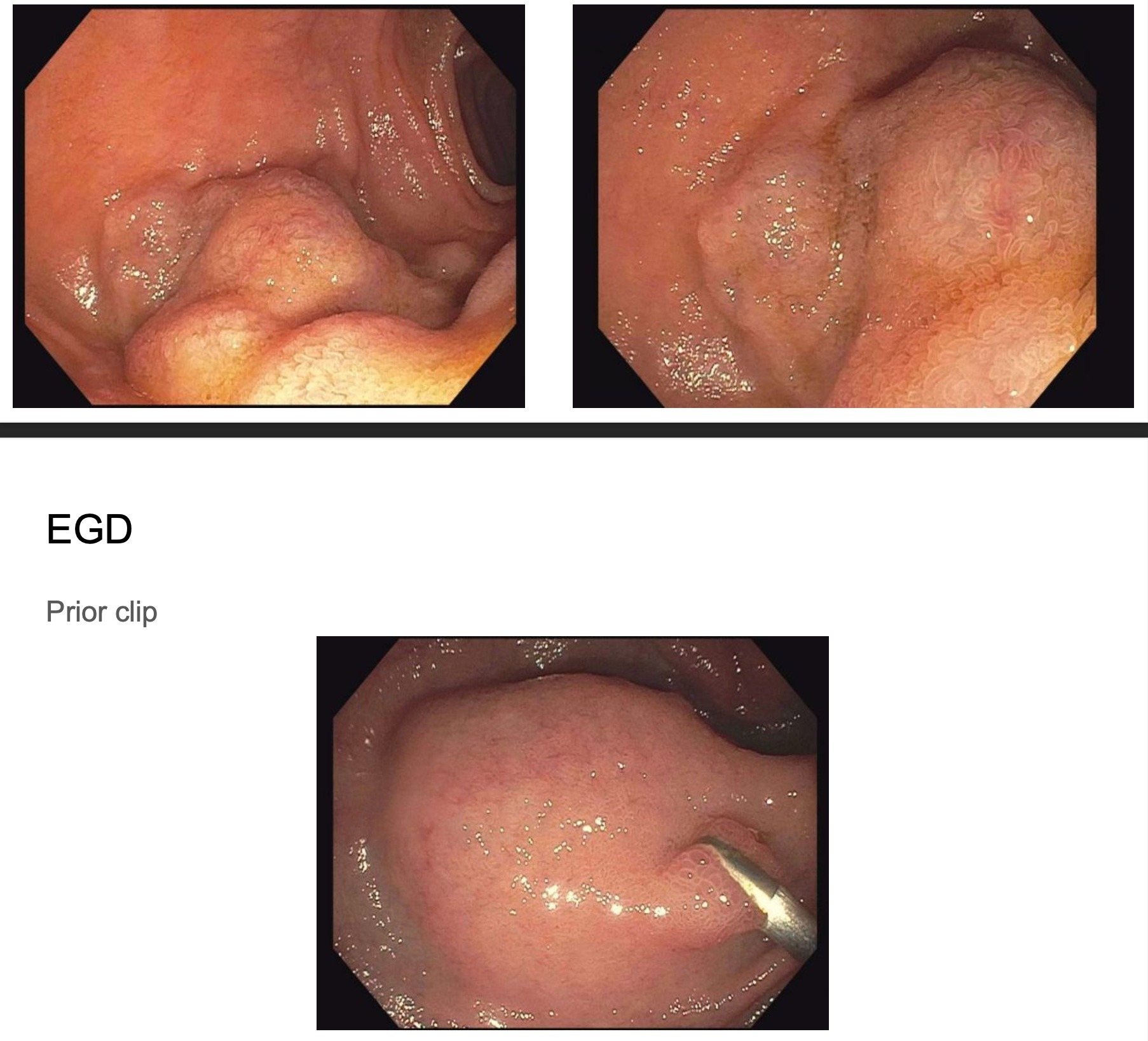
Figure: Duodenal Varices
Disclosures:
Ruona Ebiai indicated no relevant financial relationships.
Jasmine McNair indicated no relevant financial relationships.
Jordan Boudreaux indicated no relevant financial relationships.
Ravi Jariwala indicated no relevant financial relationships.
Kelli Morgan indicated no relevant financial relationships.
Ruona Ebiai, MD, Jasmine McNair, MD, Jordan Boudreaux, MD, Ravi Jariwala, MD, Kelli Morgan, MD. P2524 - Duodenal Varices as a Rare Etiology of Upper GI Bleeding in a Patient With Roux-en-Y Gastric Bypass Anatomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
