Monday Poster Session
Category: GI Bleeding
P2526 - Pill to Peril: The Hidden Impact of OCPs
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- EC
Evan Conder
University of Kentucky College of Medicine
Louisville, KY
Presenting Author(s)
Evan Conder, 1, Yan Chu, MD2, Eun Lee, MD3, Marijeta Pekez, MD4
1University of Kentucky College of Medicine, Louisville, KY; 2University of Kentucky College of Medicine, Lexington, KY; 3University of Kentucky, Georgetown, KY; 4University of Kentucky, Lexington, KY
Introduction: A 20-year-old previously healthy female presented with sudden onset lower abdominal cramping, diarrhea and hematochezia for one day. She had chills, nausea and decreased appetite. There was no significant surgical, social or family history. Her only medication was norgestimate and ethinyl estradiol, with no recent antibiotic or NSAID use.
Case Description/Methods: Patient was stable with a normal abdomen and external hemorrhoids on exam. She had leukocytosis, elevated fecal calprotectin, but normal hemoglobin, CRP, lactate and infectious workup. CT showed wall thickening and decompression of the distal transverse, descending and proximal-mid sigmoid colon, concerning for colitis.
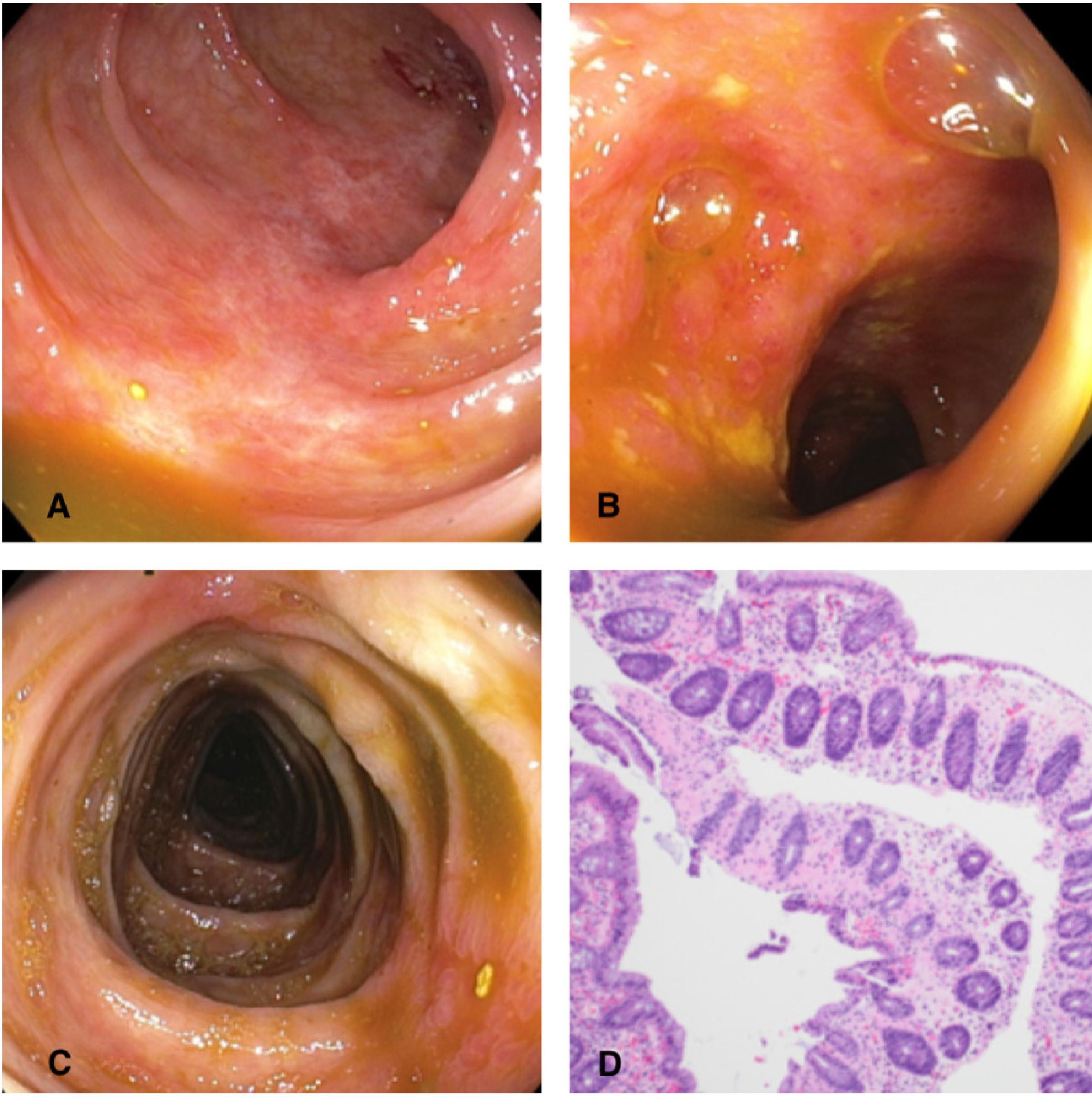
There was high suspicion for UC given her age and presentation. Colonoscopy showed normal terminal ileum, but congested, granular and linear erythematous mucosa suggesting ulceration in the transverse through descending colon. Biopsies of the ascending and descending colon were unremarkable. In contrast, the transverse colon biopsy revealed areas of coagulative ischemic type necrosis. She significantly improved with discontinuation of OCPs and supportive care.
Discussion: Patient’s age and symptoms were initially suggestive of IBD. Ischemic colitis was low on the differential, as it classically occurs in older adults with cardiovascular diseases, thrombotic disorders or other conditions that reduce intestinal blood flow. These patients can similarly present with abdominal pain, diarrhea and hematochezia. Major risk factors for ischemic injury were absent in this young, previously healthy woman. Interestingly, she was taking a combined estrogen-progesterone OCP.
Estrogen in OCPs is known to cause venous thrombosis. However, only a few case reports exist on ischemic colitis associated with OCPs. Any part of the colon can be affected, but around 75% involved left colon, 25% included splenic flexure1. Ischemic colitis may be overlooked in the absence of obvious atherosclerotic risk factors in young women. Although rare, OCP induced colitis should be considered, as they remain the most prevalent method of contraception. While CT helps to exclude diseases of similar presentation, colonoscopy with biopsy is instrumental in diagnosis. Most patients improve with supportive care and cessation of causative agent, but those who progress to peritonitis require surgery.
1. Seon, Choon Sik et al. “A Case of Oral-contraceptive Related Ischemic Colitis in Young Woman.” Clinical endoscopy vol. 44,2 (2011): 129-32
Disclosures:
Evan Conder, 1, Yan Chu, MD2, Eun Lee, MD3, Marijeta Pekez, MD4. P2526 - Pill to Peril: The Hidden Impact of OCPs, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Kentucky College of Medicine, Louisville, KY; 2University of Kentucky College of Medicine, Lexington, KY; 3University of Kentucky, Georgetown, KY; 4University of Kentucky, Lexington, KY
Introduction: A 20-year-old previously healthy female presented with sudden onset lower abdominal cramping, diarrhea and hematochezia for one day. She had chills, nausea and decreased appetite. There was no significant surgical, social or family history. Her only medication was norgestimate and ethinyl estradiol, with no recent antibiotic or NSAID use.
Case Description/Methods: Patient was stable with a normal abdomen and external hemorrhoids on exam. She had leukocytosis, elevated fecal calprotectin, but normal hemoglobin, CRP, lactate and infectious workup. CT showed wall thickening and decompression of the distal transverse, descending and proximal-mid sigmoid colon, concerning for colitis.
There was high suspicion for UC given her age and presentation. Colonoscopy showed normal terminal ileum, but congested, granular and linear erythematous mucosa suggesting ulceration in the transverse through descending colon. Biopsies of the ascending and descending colon were unremarkable. In contrast, the transverse colon biopsy revealed areas of coagulative ischemic type necrosis. She significantly improved with discontinuation of OCPs and supportive care.
Discussion: Patient’s age and symptoms were initially suggestive of IBD. Ischemic colitis was low on the differential, as it classically occurs in older adults with cardiovascular diseases, thrombotic disorders or other conditions that reduce intestinal blood flow. These patients can similarly present with abdominal pain, diarrhea and hematochezia. Major risk factors for ischemic injury were absent in this young, previously healthy woman. Interestingly, she was taking a combined estrogen-progesterone OCP.
Estrogen in OCPs is known to cause venous thrombosis. However, only a few case reports exist on ischemic colitis associated with OCPs. Any part of the colon can be affected, but around 75% involved left colon, 25% included splenic flexure1. Ischemic colitis may be overlooked in the absence of obvious atherosclerotic risk factors in young women. Although rare, OCP induced colitis should be considered, as they remain the most prevalent method of contraception. While CT helps to exclude diseases of similar presentation, colonoscopy with biopsy is instrumental in diagnosis. Most patients improve with supportive care and cessation of causative agent, but those who progress to peritonitis require surgery.
1. Seon, Choon Sik et al. “A Case of Oral-contraceptive Related Ischemic Colitis in Young Woman.” Clinical endoscopy vol. 44,2 (2011): 129-32
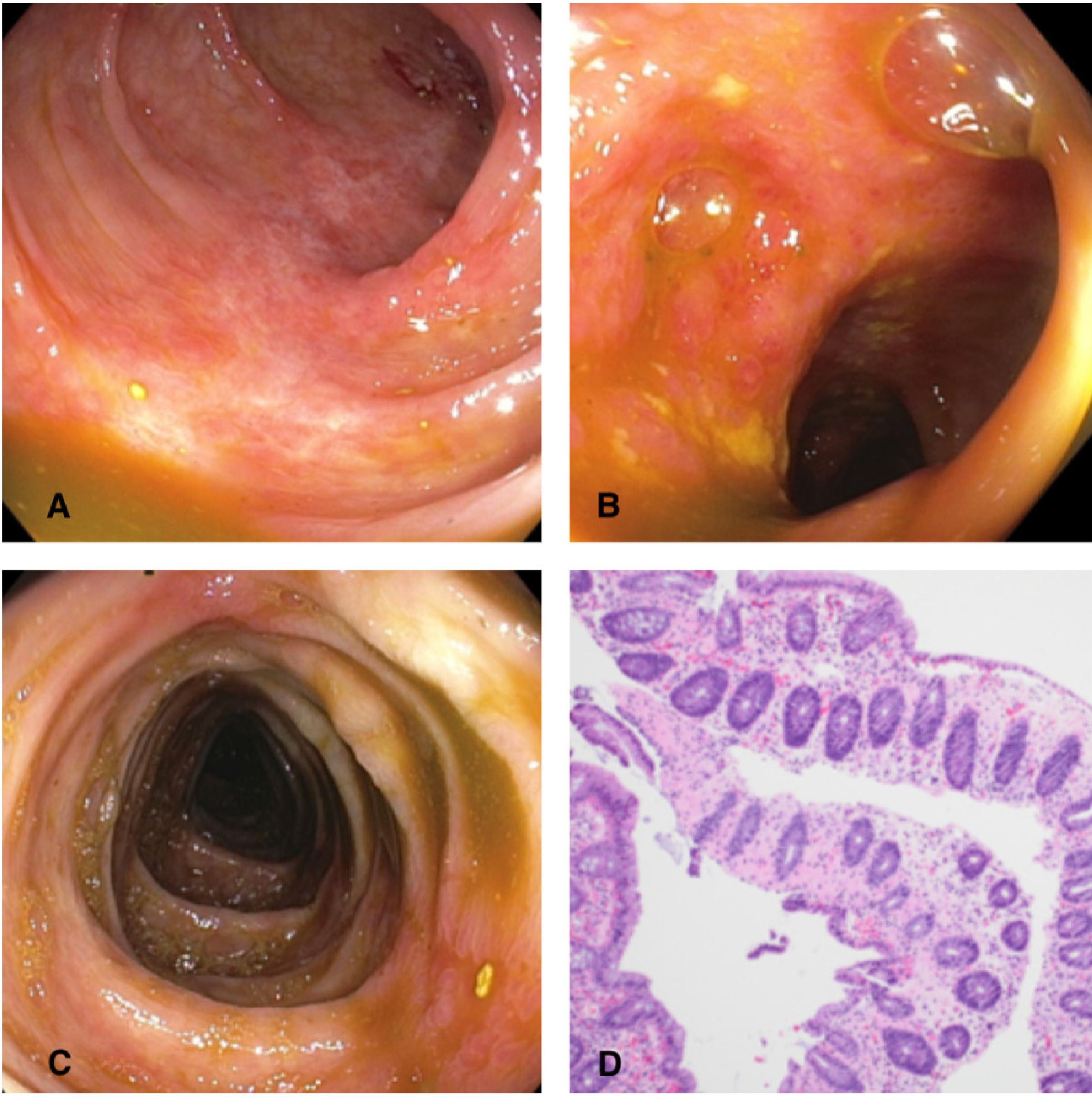
Figure: A-C: Transverse/descending colon
D: Pathology of the transverse colon biopsy showing areas of coagulative (ischemic type) necrosis (H&E stain x100)
D: Pathology of the transverse colon biopsy showing areas of coagulative (ischemic type) necrosis (H&E stain x100)
Disclosures:
Evan Conder indicated no relevant financial relationships.
Yan Chu indicated no relevant financial relationships.
Eun Lee indicated no relevant financial relationships.
Marijeta Pekez indicated no relevant financial relationships.
Evan Conder, 1, Yan Chu, MD2, Eun Lee, MD3, Marijeta Pekez, MD4. P2526 - Pill to Peril: The Hidden Impact of OCPs, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
