Monday Poster Session
Category: GI Bleeding
P2528 - Replaced Hepatic Artery: A Troublesome Anatomic Variant in a Case of Severe Upper Gastrointestinal Bleeding Refractory to Hemostatic Spray
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Clive J. Miranda, DO, MSc
CHI Health Creighton University Medical Center
Omaha, NE
Presenting Author(s)
Clive J. Miranda, DO, MSc1, Farhan Azad, DO2, Nariman Hossein-Javaheri, DO3, Bhanu Siva Mohan Pinnam, MD4, Saurabh Chandan, MD1
1CHI Health Creighton University Medical Center, Omaha, NE; 2INOVA Fairfax Hospital, Buffalo, NY; 3University at Buffalo, Buffalo, NY; 4John H. Stroger, Jr. Hospital of Cook County, Chicago, IL
Introduction: Celiac trunk (CT) anomalies have been widely studied due to their juxtaposition and contribution to the pancreas, liver, duodenum, and biliary tree. Based on the Michels Model of Classification, a type IX CT variant is described as the common hepatic artery (CHA) arising from the superior mesenteric artery (SMA), and is seen in 0.4 to 4.5% of cases. Due to its atypical site of origin, it is often termed an aberrant or a replaced hepatic artery (RHA), and is of significance in cases of refractory gastrointestinal (GI) bleeding despite endoscopic interventions.
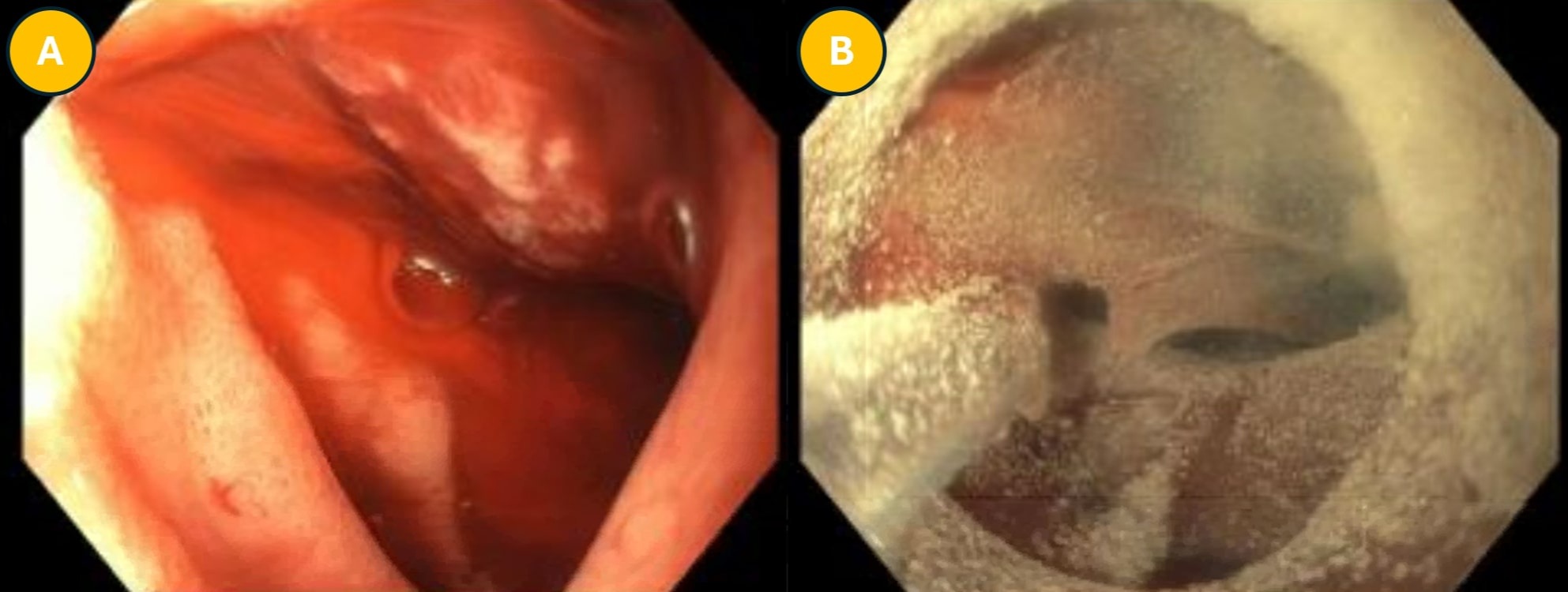
Case Description/Methods: An 80-year-old female with no prior GI history initially presented with a month of weakness and intermittent episodes of dark stool for 1 week. Hemoglobin (Hgb) was 4.6g/dL and she was given 2 units of pRBCs with repeat Hgb up to 8.7g/dL. An EGD showed a cratered duodenal ulcer with no evidence of active bleeding. The next morning, she had two more episodes of dark stool and a Hgb drop to 6.6g/dL. She then became tachycardic and hypotensive without fluid responsiveness, requiring transfer to the ICU for hemorrhagic shock. She underwent an IR-guided angiography showing a replaced CHA with frank active extravasation from the gastroduodenal artery (GDA). Despite GDA coil embolization, the patient continued to be hemodynamically unstable, requiring pressors and an additional 8 units of pRBCs. Repeat EGD showed active bleeding and a partially obstructed oozing duodenal ulcer with an adherent clot. Hemostatic spray was applied for temporary hemostasis but bleeding persisted. As the replaced CHA came off the SMA, IR was unable to re-embolize, and the patient was taken to the OR emergently for an exploratory laparotomy. She underwent a duodenotomy extending into the pyloric channel and ligation of the GDA, with primary closure via an omental patch. Upper GI series 5 days post-op showed no leak or obstruction and she was discharged a few days later with plans for repeat EGD outpatient.
Discussion: The GDA supplies the duodenum and is often a source of GI bleeding as a complication of peptic ulcer disease. RHA coming off the SMA can travel in proximity to the pancreas in several ways and can be inaccessible for arterial embolization by IR, thereby requiring emergent surgical intervention. The utility of hemostatic spray is evident in the high rates of initial hemostasis and low rates of refractory bleeding as low as 8% in patients. However, anatomic variations as seen in this case warrant a multi-disciplinary approach.
Disclosures:
Clive J. Miranda, DO, MSc1, Farhan Azad, DO2, Nariman Hossein-Javaheri, DO3, Bhanu Siva Mohan Pinnam, MD4, Saurabh Chandan, MD1. P2528 - Replaced Hepatic Artery: A Troublesome Anatomic Variant in a Case of Severe Upper Gastrointestinal Bleeding Refractory to Hemostatic Spray, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1CHI Health Creighton University Medical Center, Omaha, NE; 2INOVA Fairfax Hospital, Buffalo, NY; 3University at Buffalo, Buffalo, NY; 4John H. Stroger, Jr. Hospital of Cook County, Chicago, IL
Introduction: Celiac trunk (CT) anomalies have been widely studied due to their juxtaposition and contribution to the pancreas, liver, duodenum, and biliary tree. Based on the Michels Model of Classification, a type IX CT variant is described as the common hepatic artery (CHA) arising from the superior mesenteric artery (SMA), and is seen in 0.4 to 4.5% of cases. Due to its atypical site of origin, it is often termed an aberrant or a replaced hepatic artery (RHA), and is of significance in cases of refractory gastrointestinal (GI) bleeding despite endoscopic interventions.
Case Description/Methods: An 80-year-old female with no prior GI history initially presented with a month of weakness and intermittent episodes of dark stool for 1 week. Hemoglobin (Hgb) was 4.6g/dL and she was given 2 units of pRBCs with repeat Hgb up to 8.7g/dL. An EGD showed a cratered duodenal ulcer with no evidence of active bleeding. The next morning, she had two more episodes of dark stool and a Hgb drop to 6.6g/dL. She then became tachycardic and hypotensive without fluid responsiveness, requiring transfer to the ICU for hemorrhagic shock. She underwent an IR-guided angiography showing a replaced CHA with frank active extravasation from the gastroduodenal artery (GDA). Despite GDA coil embolization, the patient continued to be hemodynamically unstable, requiring pressors and an additional 8 units of pRBCs. Repeat EGD showed active bleeding and a partially obstructed oozing duodenal ulcer with an adherent clot. Hemostatic spray was applied for temporary hemostasis but bleeding persisted. As the replaced CHA came off the SMA, IR was unable to re-embolize, and the patient was taken to the OR emergently for an exploratory laparotomy. She underwent a duodenotomy extending into the pyloric channel and ligation of the GDA, with primary closure via an omental patch. Upper GI series 5 days post-op showed no leak or obstruction and she was discharged a few days later with plans for repeat EGD outpatient.
Discussion: The GDA supplies the duodenum and is often a source of GI bleeding as a complication of peptic ulcer disease. RHA coming off the SMA can travel in proximity to the pancreas in several ways and can be inaccessible for arterial embolization by IR, thereby requiring emergent surgical intervention. The utility of hemostatic spray is evident in the high rates of initial hemostasis and low rates of refractory bleeding as low as 8% in patients. However, anatomic variations as seen in this case warrant a multi-disciplinary approach.
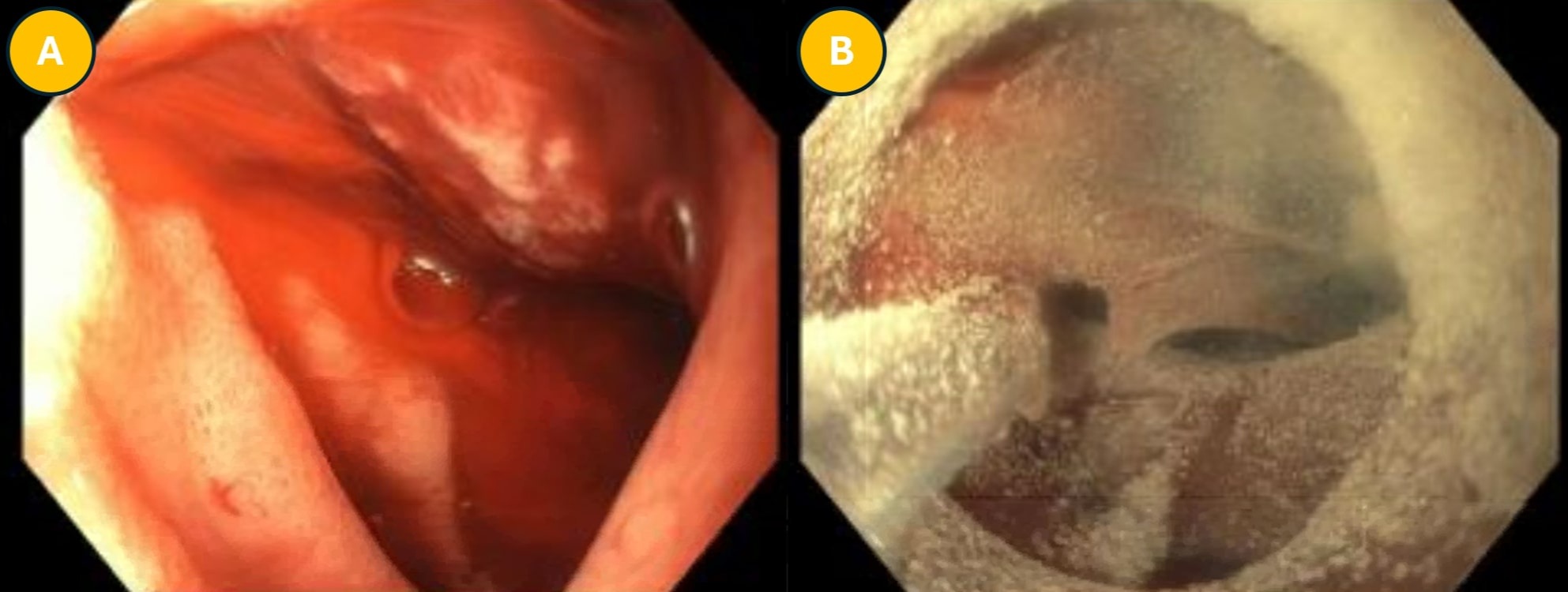
Figure: A: 2nd portion of duodenum showing partially obstructed oozing ulcer with adherent clot.
B: Duodenal bulb status-post hemostatic spray which failed to stop oozing.
B: Duodenal bulb status-post hemostatic spray which failed to stop oozing.
Disclosures:
Clive Miranda indicated no relevant financial relationships.
Farhan Azad indicated no relevant financial relationships.
Nariman Hossein-Javaheri indicated no relevant financial relationships.
Bhanu Siva Mohan Pinnam indicated no relevant financial relationships.
Saurabh Chandan indicated no relevant financial relationships.
Clive J. Miranda, DO, MSc1, Farhan Azad, DO2, Nariman Hossein-Javaheri, DO3, Bhanu Siva Mohan Pinnam, MD4, Saurabh Chandan, MD1. P2528 - Replaced Hepatic Artery: A Troublesome Anatomic Variant in a Case of Severe Upper Gastrointestinal Bleeding Refractory to Hemostatic Spray, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
